By Gustavo Gomez, MD
Data courtesy of Nucléos, Brasilia, Brazil
History
A 26-year-old female with a history of papillary carcinoma of the thyroid was treated with a total thyroidectomy with neck dissection in September 2014. The histopathology showed a 2.5 cm classic papillary carcinoma in the left lobe. Out of 96 dissected neck nodes, 36 were metastatic on histopathological examination.
The patient underwent large-dose 131I therapy (200 mCi) in December 2014. A post-therapy 131I whole-body scan showed a focal area of increased uptake in the retropharynx and cervical region. The patient suffered severe sialoadenitis following iodine therapy and was on follow-up for 10 months. The patient then underwent serum thyroglobulin assay in October 2015, which showed a high value of 32.7 ng/ml. In view of the suspicion of nodal recurrence in the thyroid bed or neck, a neck ultrasound was performed in February 2016 that revealed an enlarged level III left cervical node, which was strongly suspicious for metastasis. Surgical removal of the left cervical lymph node was performed in March 2016 and the histopathology revealed a nodal metastasis from papillary thyroid carcinoma. A diagnostic whole-body 131I scan performed in June 2016 was negative, although a repeat serum thyroglobulin performed at the same time showed persistent high values (serum thyroglobulin in June 2016 was 27.8 ng/ml). In view of the lack of 131I-avid nodal metastases, and the patient’s refusal to undergo further large-dose iodine therapy due to complications from the first therapy, plans for a second radioiodine therapy were abandoned.
Thyroid carcinoma often expresses somatostatin receptors and (111In or 99mTc octreotide) somatostatin receptor scintigraphy or PET can be positive in patients with iodinenegative thyroid carcinoma.1 Based on this consideration, the patient was referred for a 99mTc octreotide somatostatin receptor SPECT/CT in August 2016. The octreo scan images showed positive focal uptake in the retropharynx, which was suggestive of a somatostatin receptor-positive, radioiodinenegative metastases. In view of the presence of somatostatin receptorpositive retropharyngeal metastases, the patient was given four cycles of 177Lu DOTATATE therapy, each dose being approximately 200 mCi between October 2016 to June 2017.
A repeat serum thyroglobulin performed in August 2017 showed a high value of 20.6 ng/ml. The patient was subsequently referred for Fludeoxyglucose F 18 injection (18F FDG) PET/CT followed by 68Ga DOTATOC PET/CT to assess the status of the retropharyngeal metastasis and to evaluate for new lesions.
The patient was initially evaluated with 18F FDG PET/CT in August 2017 and a 68Ga DOTATOC PET/CT was performed the following day. Following intravenous (IV) administration of 7.7 mCi (287 MBq) of 18F FDG and 65 minutes postinjection delay, a whole-body PET/CT was performed using low-dose CT (110 kV, 125 ref mAs, 16 x 1.2 mm collimation, 3 mm slice thickness) followed by a PET acquisition at 2 minutes per bed position on Biograph™ Horizon. A dedicated single bed position PET/CT study for the head and neck region was subsequently performed with a low-dose CT (110 kV, 34 eff mAs, 16 x 1.2 mm collimation, 3 mm slice thickness), followed by a PET acquisition of 4 minutes. PET was acquired using time-of-flight (ToF) and an ultraHD reconstruction of PET data (a reconstruction technique combining ToF with point spread function (PSF)) was fused with CT for evaluation of both whole-body and dedicated head-and-neck PET/CT. PET/CT using 68Ga DOTATATE was performed the following day. One hour following administration of 3.3 mCi (125 MBq ) of 68Ga DOTATOC, a low-dose whole-body CT (110 kV, 125 ref mAs, 16 x 1.2 mm collimation, 2 mm slice thickness) was followed by a whole-body PET acquisition at 3 minutes per bed. A dedicated single bed position PET/CT study for the head and neck region was also acquired with a protocol similar to that of the 18F FDG study.
Findings
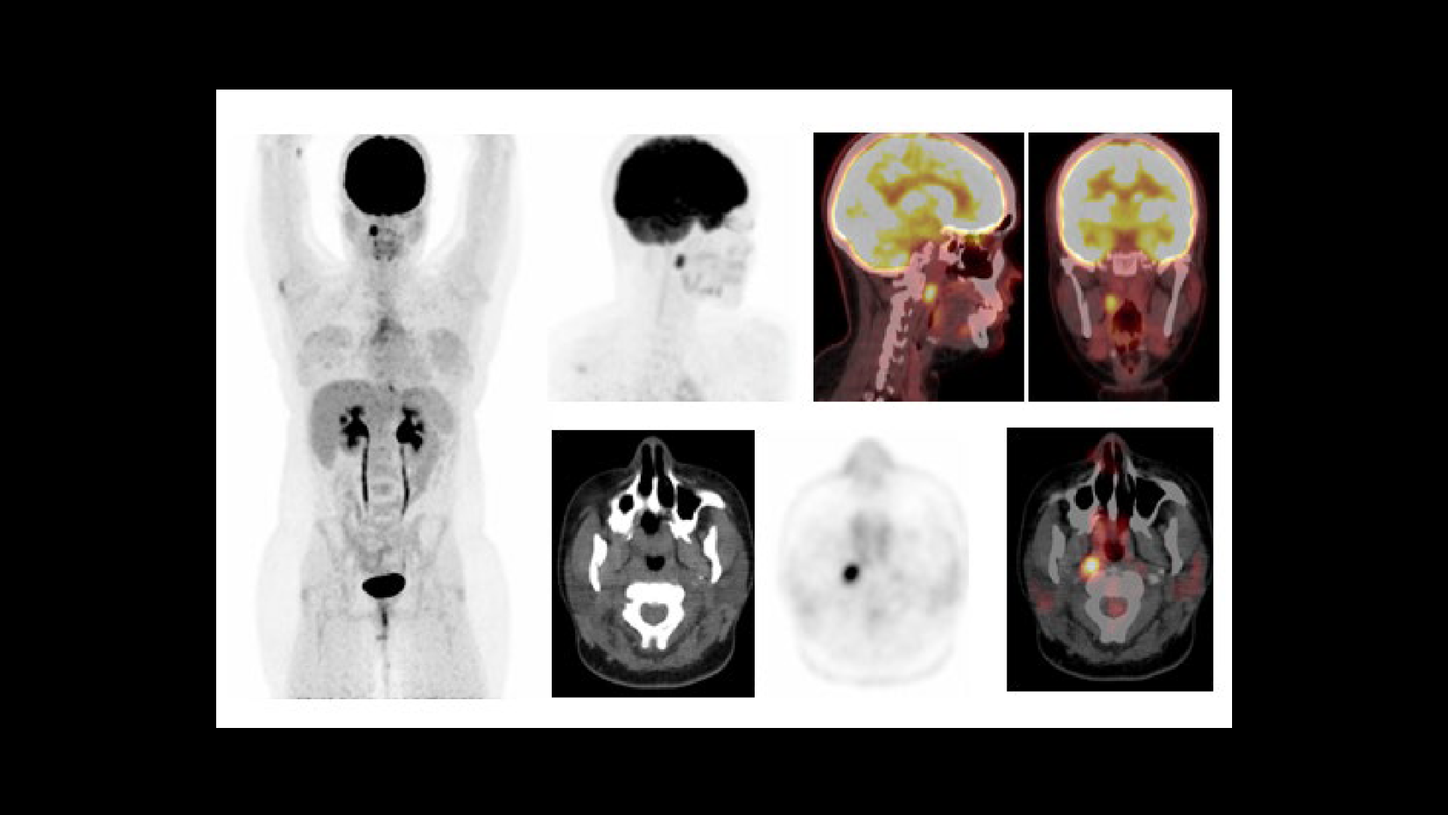
As shown in Figure 1, an increased glucose metabolism in the right palatine tonsillar mass is suggestive of a glucose-avid metastasis from papillary carcinoma of the thyroid, which corresponds to the lesion previously delineated on the 99mTc octreotide somatostatin receptor scintigraphy.
68Ga DOTATOC PET/CT (Figure 2) correlates with the diagnosis of a pharyngeal somatostatin receptorpositive, radioiodine-negative metastasis originating from papillary thyroid carcinoma, based on the previous somatostatin receptor scintigraphy.
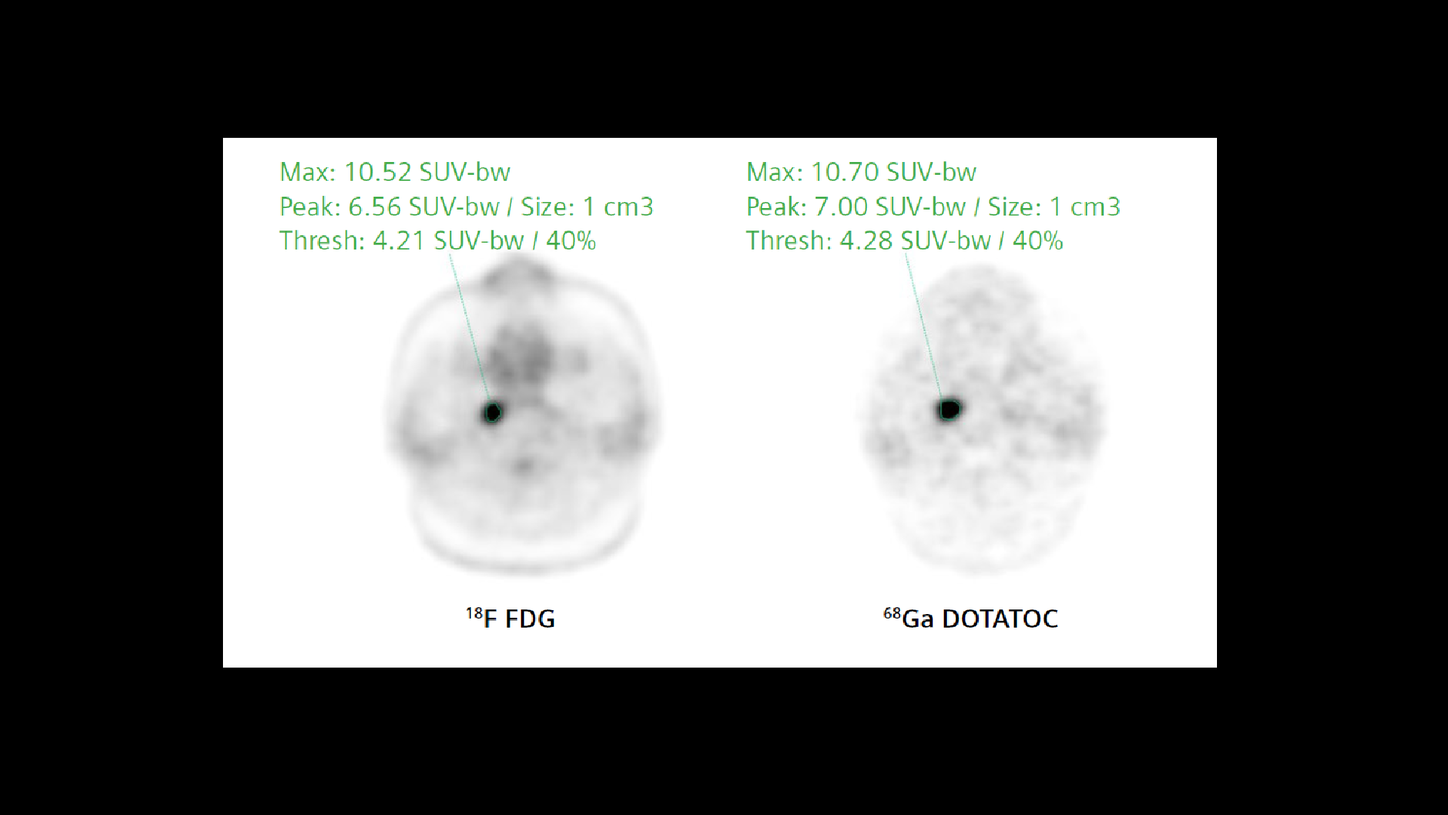
As seen in Figures 1 and 2, as well as the comparison of 18F FDG and 68Ga DOTATOC uptake within the pharyngeal metastasis, the lesion shows a similar high level of uptake of both tracers that is possibly suggestive of an aggressive, poorly differentiated glucose-avid metastasis with significant somatostatin receptor positivity. The high level of 68Ga DOTATOC uptake even after four previous therapy cycles of 177Lu DOTATATE opens up the possibility of further therapy cycles.
The patient underwent a follow-up scan again in July 2018 and the serum thyroglobulin was measured at 17.4 ng/ml, which was slightly lower than the value measured in August 2017. The patient also underwent 18F FDG and 68Ga DOTATOC PET/CT studies with a similar acquisition protocol as the previous study. Both 18F FDG and 68Ga DOTATOC PET/CT studies showed the presence of the pharyngeal metastasis with slightly lower SUVmax (18F FDG SUVmax 7.9 and 68Ga DOTATOC SUVmax 8.9) as compared to the previous study. No new metastases were visualized. The slight reduction of serum thyroglobulin and lesion SUVmax is a possible effect of the previous radionuclide therapy with 177Lu DOTATATE.
Comments
Although differentiated thyroid carcinoma is usually 131I-avid and can be effectively treated with radioiodine, some metastatic lesions become dedifferentiated and lose their capacity to accumulate radioiodine. 18F FDG PET/CT has been shown to be sensitive in the detection of radioiodinenegative metastases in differentiated thyroid carcinoma with elevated serum thyroglobulin levels. The sensitivity of 18F FDG PET/CT increases with
stimulated Tg levels and reaches 100% sensitivity at stimulated Tg > 28.5 ng/ml.2 Thyroid carcinoma expresses somatostatin receptors and (111In-octreotide) somatostatin receptor scintigraphy has shown high sensitivity in the detection of radioiodinenegative thyroid carcinoma metastases.1 Expression of somatostatin receptors in thyroid carcinoma cells is the rationale behind usage of 68Ga DOTATOC PET/CT for the detection of somatostatin receptorpositive thyroid carcinoma metastases, particularly for radioiodine-negative metastases, which often pose a diagnostic challenge.
A study compared 18F FDG PET to 68Ga DOTATOC PET in a series of 17 patients with differentiated thyroid cancer.3 Out of 104 malignant lesions, 18F FDG PET showed an only slightly higher detection rate than 68Ga DOTATOC PET in radioiodinepositive lesions (28/31 versus 25/31), whereas 18F FDG was significantly more sensitive in radioiodine-negative metastatic lesions (70/73 versus 26/73). Three out of 104 lesions were visible using 68Ga DOTATOC PET only.
Although this study shows 18F FDG PET to have a higher sensitivity compared to somatostatin-receptor PET in radioiodine-negative thyroid cancer, studies show the value of 68Ga DOTATOC PET in the detection of thyroid carcinoma metastases, which were radioiodine negative as well as 18F FDG PET negative.4 In this study, 68Ga DOTATOC was positive in 33% of patients who had metastases that were radioiodine and 18F FDG negative where most of these lesions were poorly differentiated. The rate of somatostatin receptor positivity in 18F FDG and radioiodine negativedifferentiated papillary and follicular carcinomas was lower.
Somatostatin receptor positivity in 111In octreotide SPECT and 68Ga DOTATOC PET in patients with radioiodine-negative thyroid carcinoma metastases has lead to therapy options using somatostatin receptor-seeking therapeutic radiopharmaceuticals like 177Lu DOTATATE. Elboga et al. performed radionuclide therapy with two cycles of 200 mCi of 177Lu DOTATATE in a patient with 18F FDG- and 68Ga DOTATOC-positive metastases in the lung, mediastinal lymph node, ribs, and muscle with a significant decrease in serum Tg
(609 ng/ml pre therapy to 9 ng/ml after 200 mCi 177Lu DOTATATE therapy cycles) after two cycles.5
Conclusion
The present case highlights the synergy that may be achieved by combining 18F FDG and 68Ga DOTATOC PET/CT in patients with elevated thyroglobulin and negative radioiodine whole-body scans. Although 18F FDG PET/CT detected the hypermetabolic pharyngeal metastasis with high contrast, the high uptake of 68Ga DOTATOC with SUVmax levels similar to that of 18F FDG suggested the need to continue 177Lu DOTATATE therapy. The follow-up PET/CT study performed in July 2018 demonstrated a decrease in lesion SUV for both 18F FDG and 68Ga DOTATATE PET/CT with no fresh metastatic lesion, which reflects the effect of previously delivered radionuclide therapy.
In a patient where all other therapy options were exhausted or rejected by the patient due to toxicity concerns, 177Lu DOTATATE therapy offered an alternative, which led to a slight decrease in serum thyroglobulin as well as a significant reduction in lesion uptake, as evident in the follow-up study.