By Samart Rajchadara, MD and Ananya Ruangma, PhD
Data courtesy of Bangkok General Hospital, Bangkok, Thailand
History
A 38-year-old female presented with a left breast mass, which initially proved to be benign following an examination and aspiration biopsy. However, during the clinical examination, a nodule in the right lobe of the thyroid was palpated. An ultrasonography of the thyroid was therefore performed and revealed 3 calcified nodules in the right lobe of the thyroid along with a small cystic nodule at the upper pole of the right lobe. The ultrasonography also demonstrated enlarged lymph nodes at the superior aspect of both jugular chains. A fine needle aspiration biopsy of the right thyroid nodules was performed under ultrasound guidance and a cytology revealed papillary thyroid carcinoma coexisting with nodular goiter.
In view of the diagnosis of papillary thyroid carcinoma, the patient underwent a near total thyroidectomy. A histopathology of the surgical specimen confirmed the diagnosis of encapsulated papillary microcarcinoma of the right lobe without capsular or vascular invasion. Due to high serum thyroglobulin (Tg), the patient was referred for high-dose radioiodine therapy for ablation of residual thyroid, where 100 mCi of 131I was administered. A post-therapy 131I whole-body scintigraphy (Figure 1) showed expected high 131I uptake of the residual thyroid in the neck but had no clearly defined iodine-avid metastases. The radioiodine uptake in the stomach and bowels were within physiological limits.
Six months post-131I large dose therapy, the patient underwent a follow-up Tg and 131I whole-body planar scan. The whole-body radioiodine scan (Figure 2) did not show 131I uptake in the neck, thus suggesting that the post-surgery residual thyroid tissue was ablated. There were no other functioning metastases and the colonic uptake of the tracer was within physiological limits.
Although the follow-up 131I whole-body scan was negative, the Tg was high, which suggested the possibility of radioiodine negative metastases or recurrence. Since radioiodine negative thyroid carcinoma recurrences are often poorly differentiated and 18F FDG-avid, the patient underwent a Fludeoxyglucose F 18 injection (18F FDG) PET/CT scan.
The study was performed on a Biograph mCT Flow™ with FlowMotion™. Ninety minutes following an IV injection of 10 mCi of 18F FDG, the PET/CT study was performed with a whole-body contrast CT (120 kV, 222 eff mAs). Thereafter, the PET acquisition used continuous bed motion with a uniform table speed of 1 mm/sec as well as ultraHD•PET (time-of-flight with point-spread function (PSF) reconstruction). The reconstructed PET, contrast CT, and fused PET/CT images were evaluated for clinical reporting.
Findings
The 18F FDG PET/CT scan (Figures 3 and 4) revealed 18F FDG-avid recurrent thyroid carcinoma lesions in the neck, which were found within the lower thyroid bed adjacent to, anterior to, and lateral to the trachea. Hypermetabolic upper cervical lymph node metastases on both sides of the neck were also clearly delineated and especially prominent in the high resolution PET reconstruction of the head and neck region.
In view of the diagnosis of 18F FDG-avid radioiodine negative recurrent disease in the neck and the bilateral lymph node metastases, the patient underwent further surgery to remove the recurrent lesion and the lymph nodes in the neck.
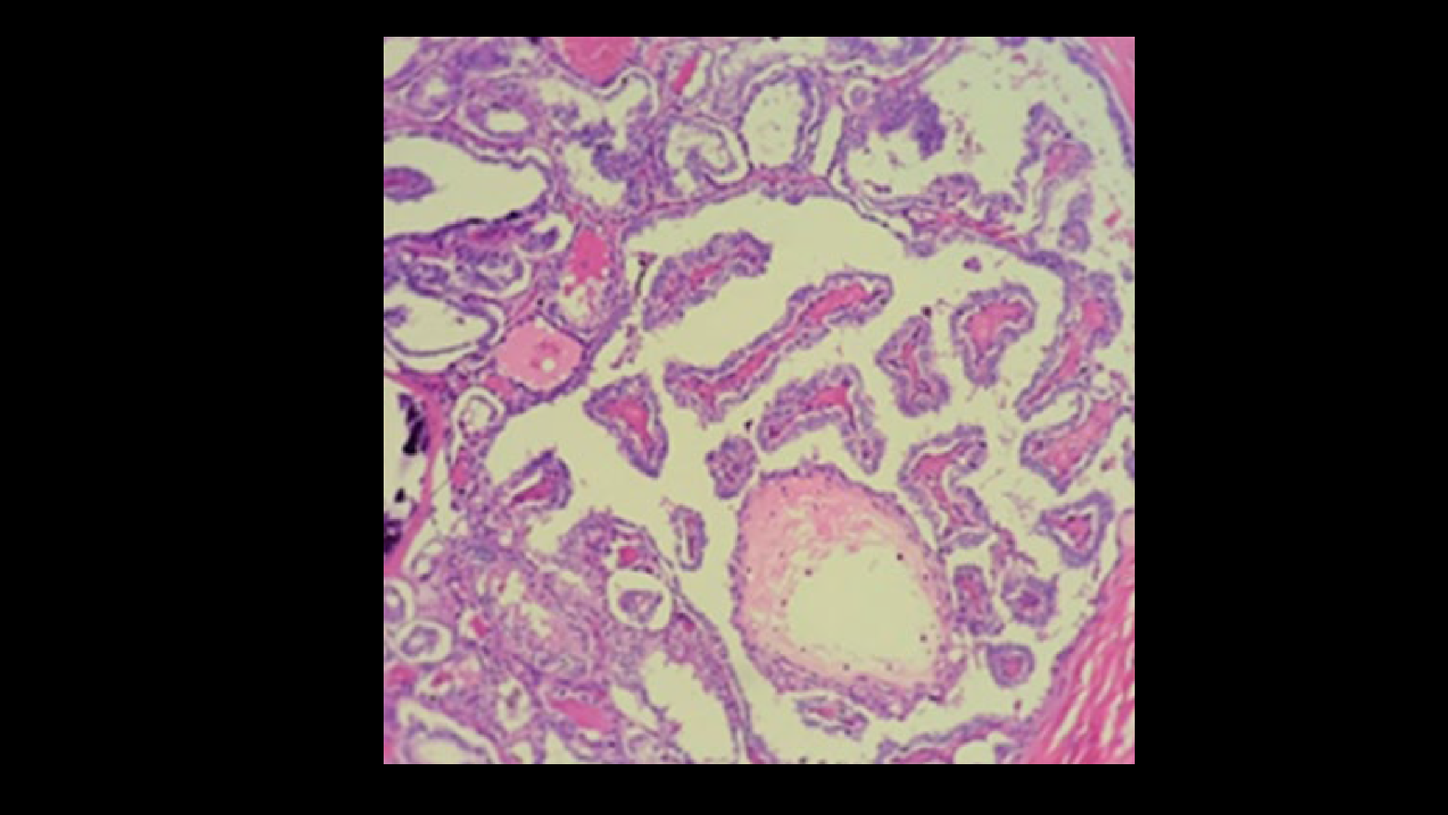
A histopathology of the resected recurrent nodules (Figure 5) and upper cervical lymph node metastases removed from along the internal jugular vein demonstrated presence of papillary thyroid carcinoma.
Comments
Differentiated thyroid carcinoma is usually treated by total thyroidectomy and radioactive iodine ablation therapy and during follow-up. An elevated Tg concentration is a sensitive marker indicating persistent or recurrent disease and is usually associated with positive 131I whole-body scan findings. Some patients, however, have metastases that do not concentrate 131I (even when it is given in therapeutic doses). Metastases that are unable to concentrate 131I are usually poorly differentiated with an impaired ability to trap iodine and are often more aggressive clinically. 18F FDG PET/CT has demonstrated high sensitivity for detection of thyroglobulin positive, radioiodine negative, recurrent or metastatic thyroid carcinoma. In a study, 18F FDG PET was performed in 37 patients with thyroid carcinoma post total thyroidectomy who showed elevated Tg with negative 131I whole-body scans.1 18F FDG PET was positive in 76% (28/37) of these patients and accurately localized 89% of the lesions. A change in management secondary to PET was predominantly surgical resection of recurrent lesions or external radiation therapy in a smaller group.
Although the majority of recurrent or metastatic thyroid carcinoma lesions with high Tg are also radioiodine-avid (and thus successfully treatable with a high dose of 131I therapy), a small percentage show low iodine uptake but high 18F FDG uptake. In 49 post-thyroidectomy cancer patients who had persistently elevated serum Tg following initial radioiodine ablation, Salvatore et al. performed 18F FDG PET/CT immediately prior to empirical high dose 131I therapy.2 In 9 of the 49 patients (18%), 18F FDG PET/CT was positive while 131I whole-body planar imaging was negative. Conversely, in a similar percentage of patients, 18F FDG PET/CT was negative and 131I whole-body planar imaging was positive. Following an empirical high-dose 131I radioiodine therapy, Tg levels remained unchanged or increased in a larger number of patients with positive 18F FDG PET/CT scans compared to those with negative 18F FDG PET/CT scans. The patients with positive PET/CT (76%) did not have a significant decrease in Tg following empirical radioiodine ablation, although ablation results were superior in patients who were FDG negative and radioiodine positive.
Conclusion
In the present case, a histopathology following an initial surgery revealed papillary microcarcinoma without capsular or vascular invasion and thus was suggestive of a good prognosis. However, very high Tg following thyroidectomy was an indication of a potentially aggressive tumor, which led to the decision for high-dose radioiodine ablation therapy. Although a follow-up diagnostic 131I whole-body scan showed no evidence of residual thyroid or metastases, persistently increasing Tg raised the suspicion of poorly differentiated non-iodine-avid recurrence, which was confirmed with an FDG PET/CT scan. High-resolution reconstructions of the PET/CT enabled sharp high contrast delineation of bilateral upper cervical lymph node metastases with low level of FDG uptake, which indicated nodal spread. The PET/CT appearance of multiple paratracheal recurrent thyroid carcinoma nodules with hypermetabolic upper cervical lymph nodes on both sides of the neck and the possibility of multiple neck nodal micrometastases led to surgical excision of recurrent nodules as well as bilateral lymph nodal resection. A histopathology subsequently confirmed presence of papillary thyroid carcinoma within recurrent nodules and some lymph nodes. Empirical high-dose 131I therapy in patients who are Tg positive but 131I diagnostic whole-body scan negative have shown mixed results with 63% of patients achieving a decrease in Tg following therapy and post-high-dose 131I therapy scans, thus demonstrating recurrence or metastases in 62% of patients.3 Studies have also shown the efficacy of tyrosine kinase inhibitors, such as Lenvatinib, in radioactive iodine refractory metastatic thyroid cancer.4 Although clear delineation of 18F FDG-avid metastases (which do not show radioiodine avidity in the present situation) make a clear case for surgical excision, close Tg follow-up is an absolute necessity.