In radiation therapy simulation and planning, Magnetic Resonance Imaging (MRI) provides superior soft tissue contrast and has become the gold standard for imaging prostate, brain, liver, head and neck tumors, showing improvements in target delineation accuracy. This capability can inform treatment planning and delivery accuracy. Having a dedicated MRI can bring these improvements closer at hand, streamlining your workflows and improving patient experiences.
Investing in a dedicated MRI system within a radiation oncology department streamlines patient care, reduces the need for external referrals, and helps ensure immediate access to critical imaging. While ordering MRI scans can still provide better soft tissue images for simulation and planning, referring patients presents challenges, too. Without a dedicated MRI unit, scheduling can be more complicated, often leading to delays in obtaining critical imaging needed for diagnosis and treatment planning. Patients may face longer wait times and must travel to a different location and meet different staff, which adds stress and disrupts their treatment flow. For staff, coordinating external imaging with radiotherapy planning can introduce workflow inefficiencies, increase administrative burdens, and create the potential for registration errors between CT and MRI scans. This lack of integration can lead to less-precise treatment, requiring more-invasive methods to ensure target accuracy and ultimately compromising the overall patient experience and delaying treatment.
The benefits of a dedicated MRI for radiation therapy
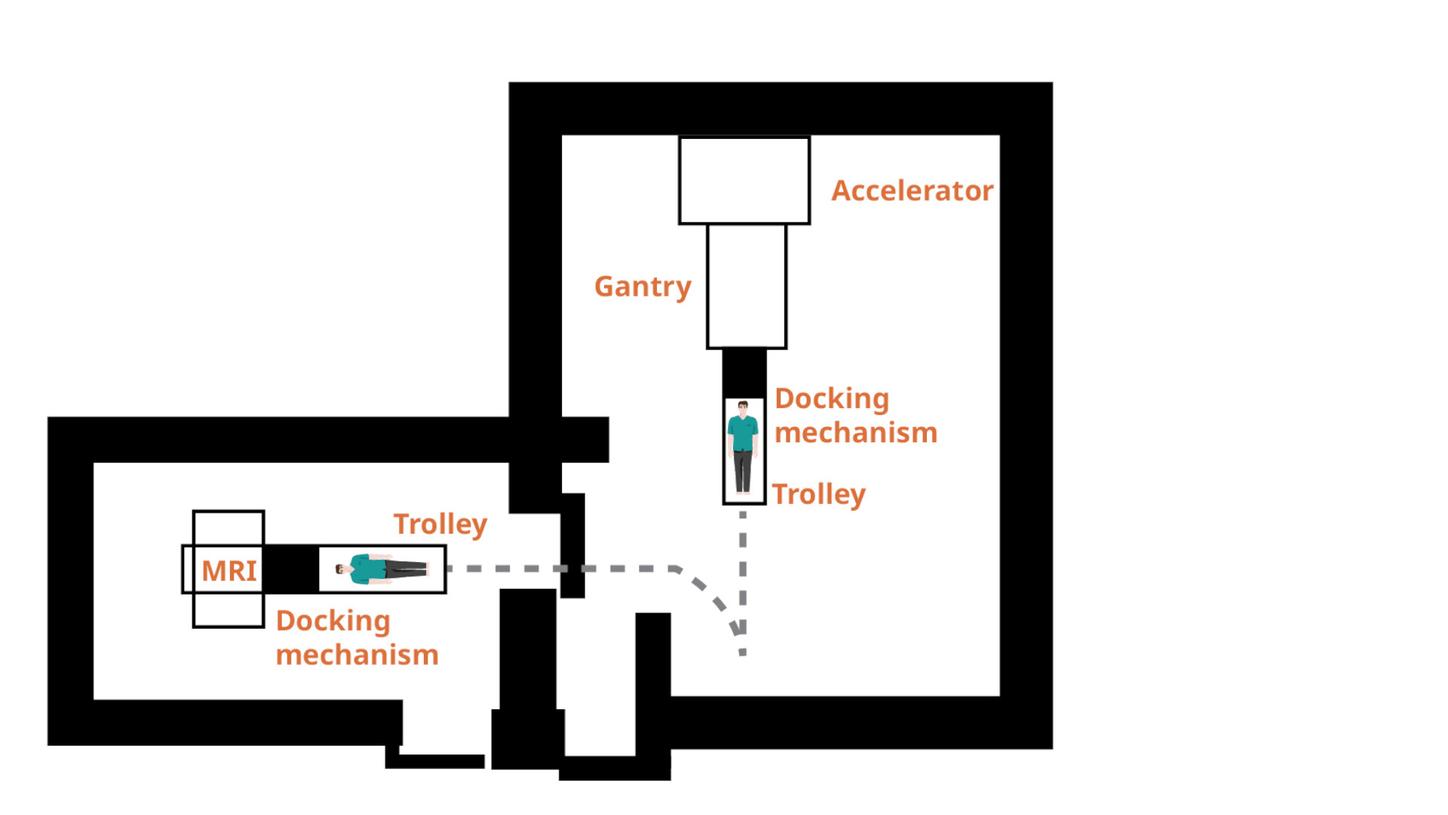
Better workflow: Adding MRI specifically for radiation therapy provides control over the system and imaging protocols as well as physical proximity to treatment devices. One hospital found that installing a 1.5T MRI system close to a linear accelerator and using a special trolley to transport patients between the two revolutionized the treatment flow. The patients were already positioned, and this made the transition from simulation to treatment faster and easier. By using MRI only, the hospital found that they were able to avoid registration errors between CT and MRI scans. This not only streamlined the patient-setup workflow, but also reduced the need for more-invasive methods where errors previously occurred.1
Easier scheduling: Having a dedicated MRI system within the radiation therapy department means fewer scheduling hassles. Instead of waiting days (or weeks) to get a patient scanned and then to receive images, MRI scans can be done as close to treatment as possible, even the same day. By capturing the most recent, most accurate status of the tumor, treatment can be altered to provide better clinical outcomes for the patient.
Streamlined patient experience: Since the patient doesn’t need to be sent to an imaging center or radiology department, the patient can have a smoother, more integrated experience. There are fewer logistical challenges, including appointment scheduling hassles with a new office. Plus, having a dedicated MRI system means more control in positioning patients with care to get exactly the image needed, reducing possible patient discomfort or the need for repeat scans.2 The patient, and any caregivers or family members, don’t need to visit a new office—they have the advantage of familiarity with the location and the team who knows their case best.
The challenges of adding a dedicated MRI system
Having a dedicated MRI system is not without challenges. The cost, space, and infrastructure requirements needed to obtain an MRI system are a few of the initial hurdles, and even after getting a MRI unit in place, challenges may exist. For instance, in 2016, a major North American radiotherapy program installed two dedicated wide-bore MRI systems, beginning a gradual rollout of MR-based planning for treatment sites like the CNS and gynecologic areas, and in 2023, a report highlighted several challenges the program faced. A significant barrier was the shortage of radiation therapists skilled in clinical MRI applications, with most training programs still focused on CT. Over 90% of the staff lacked MRI expertise, and both therapists and radiation oncologists needed specialized training in MRI safety, image interpretation, and contouring for treatment plans.2 The report also noted common patient-related issues such as claustrophobia, discomfort during long scans, and complications from internal medical devices also posed challenges.2 Partnering with experts early in the planning process can help mitigate these challenges.
Opportunities with a dedicated MRI system in RT
Financial: A dedicated MRI system for radiotherapy improves financial efficiency by enabling more-precise treatment planning, reducing costly rescans and/or revisions to the treatment plan, and increasing patient throughput with quicker imaging and treatment starts. It minimizes radiation-related risks and long-term complications, helping to prevent additional healthcare costs. Additionally, offering advanced MRI services can attract more referrals, boosting revenue from high-precision treatments.
Adaptive planning: An in-house system provides the opportunity to add MRI-based offline and online adaptive to the department. Immediate access and control of the MRI system makes adaptive planning much more achievable, such as providing quicker data transfer and more-flexible scheduling and designing an appropriate workflow.
MRI-based adaptive radiotherapy can be especially helpful since, unlike CT, which has limitations in gross tumor volume (GTV) delineation, MRI’s superior soft tissue contrast enhances target accuracy and helps avoid geometric misses.3-6 This precision is especially critical for pediatric patients, as MRI eliminates radiation exposure while allowing for close monitoring of treatment responses.7 In offline adaptive planning, MRI’s flexible slice orientation improves anatomical alignment, reducing registration errors commonly seen when combining CT and MRI scans.7
Conclusion
As radiation oncology continues to evolve, integrating a dedicated MRI system into your practice offers undeniable advantages. MRI’s superior soft tissue contrast, precision in tumor delineation, and ability to reduce treatment margins make it an invaluable tool for improving patient outcomes. Beyond image quality, having an in-house MRI system provides its own benefits. Practices can streamline workflows, more easily incorporate adaptive treatment planning practices, and eliminate treatment delays referring patients to imaging partners. A dedicated MRI system in RT also gives you the benefits of MR images that are RT-optimized and tailormade protocols to the needs of RT for treatment planning. It also enables reproducible patient positioning and imaging during the course of the treatment/fractionations. These long-term benefits make investing in a dedicated MRI unit a strategic choice for forward-thinking radiation oncology practices.