
Cardiac Molecular Imaging: Overview
Cardiac Molecular Imaging using either SPECT or PET techniques is established since decades for myocardial perfusion diagnosis. Its clinical value is well evaluated. Cardiac stress myocardial perfusion SPECT or PET is indicated in symptomatic patients with at least an intermediate likelihood of CAD, for preoperative evaluation of patients with high risk for CAD and for follow-up of known CAD.

Cardiac Molecular Imaging: Myocardial perfusion studies
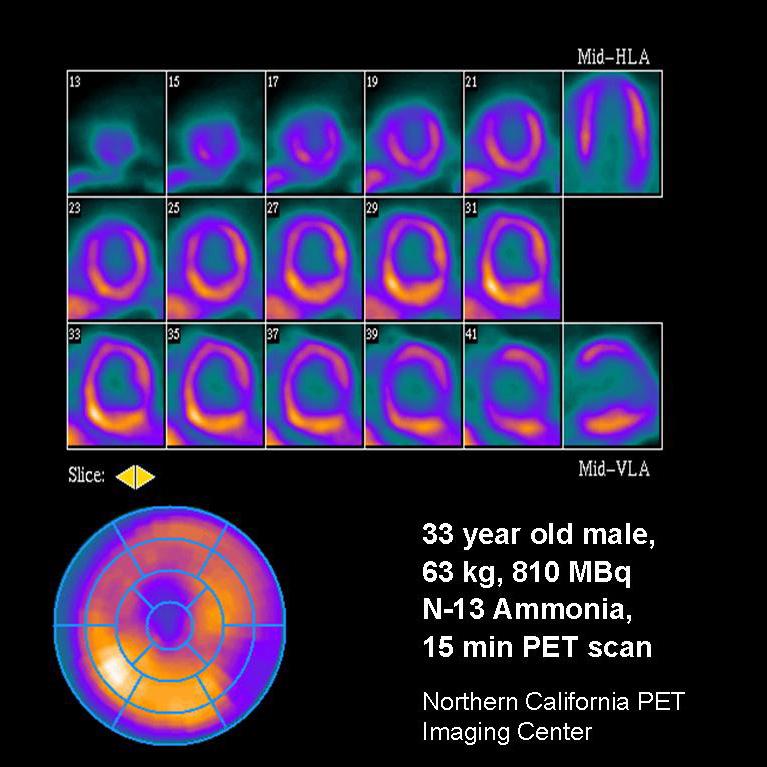
MPS with SPECT (gated or ungated) are the commonly used and well evaluated non-invasive imaging method for analysis of myocardial perfusion. The prognostic significance of MPS is well studied and documented. Different agents may be used: thallium, Tc-99m sestamibi or tetrofosmin. Innovations like IQ•SPECT drastically reduce exam time while increasing diagnostic accuracy. PET uses NH3 or rubidium as imaging agents for assessment of myocardial perfusion. In contrast to SPECT, PET allows absolute quantification of myocardial perfusion.
Cardiac Molecular Imaging: Diagnostic accuracy
The diagnostic accuracy of MPS stress testing relates to the detection of significant CAD and depends on the stressor used. Sensitivity varies between 85 and 90 % and specificity ranges from 66 to 85 %. Adenosine offers high sensitivity (90%) and specificity (85%) and is therefore the preferred stressor. Alternatives are dipyridamole, dobutamine or exercise (Myocardial perfusion scintigraphy: the evidence1). Incremental diagnostic value is added to nuclear studies when combined with functional assessments of LV ejection fraction and EDV from gated SPECT or gated PET measurements.
The latest generation SPECT•CT systems make it possible to combine CT calcium scoring and myocardial perfusion SPECT for enhanced risk stratification and higher specifity.
Cardiovascular MR: Overview
Over the last years cardiovascular MR (CMR) has proven, in many clinical studies, that it may be a valuable alternative in the evaluation of myocardial perfusion². In Stress Perfusion MRI, exam protocols are mostly identical to the ones used in nuclear cardiology, i.e. adenosine and dipyridamole are used as vasodilators. Images are acquired during the injection of the vasodilator and myocardial first-pass of a Gadolinium MR contrast agent. The diagnosis can be made either by visual assessment of the perfusion images or by a semi-quantitative analysis using post-processing tools such as ARGUS Dynamic Signal. The diagnostic accuracy of CMR compares to that of nuclear imaging3). Additional viability imaging is performed to detect scar tissue and to increase the diagnostic performance of the exam.
Cardiovascular MR: Diagnostic accuracy
For high diagnostic accuracy high temporal resolution of CMR perfusion imaging is essential. Siemens’ Tim technology offers high iPAT factors in all 3 dimensions together with 32 channel architecture for the best possible image resolution, either spatial or temporal, or a mix of both.
In the time of increasing obesity MAGNETOM Espree‘s wide bore design (ca. 70 cm) in combination with a short magnet (ca. 125 cm) makes Cardiovascular MRI also accessible for obese patients and patients feeling discomfort in normal bore scanners.

Echocardiography: VVI
Wall thickness and myocardial contractility are routinely evaluated in echo examinations of the left ventricle. Stress echo both with physical exercise or pharmacological exercise provide resting and stress induced wall motion information. Wall segments that demonstrate contraction are viable. Contrast agents and syngo VVI can aid in improving echo visualization and diagnosis in the technically difficult to image patient.
Echocardiography: MCI
Myocardial contrast echocardiography (MCE) utilizes contrast agent in order to assess myocardial perfusion in real time. MCE’s portability, rapid acquisition and interpretation of image data combined with the absence of radiation exposure make it an ideal bedside technique4). Myocardial perfusion quantitative analysis is an emerging application within echocardiography.

Cardiovascular CT
Cardiovascular CT may add additional information besides evaluation of coronary status and cardiac function: Assessment of myocardial perfusion by means of CT is based on the kinetics of iodinated contrast agent. Similar to MRI, CT data are acquired after iv administration of the contrast agent. As a result, hypoperfused myocardial regions are identified as areas displaying hypoattenuation. Continuous measurement of attenuation values allows differentiation between infarcted and viable myocardium. Further advancements may be demonstrated when using Dual Source CT with Dual Energy for diagnosing coronary artery stenosis and myocardial ischemia5).
External Links
- 1) Underwood SR et al., European Journal of Nuclear Medicine and Molecular Imaging 2004:31, 261-269
- 2) Watkins S et al., Heart 2007;93:7-10
- 3) Cheng AS et al., J Am Coll Cardiol. 2007 ;49(25):2440-9
- 4) Hayat S et al., European Heart Journal (2008) 29, 299-314
- 5) Ruzsics B et al., Eur Radiol. 2008 Jun 4. [Epub ahead of print]
Legal Information
A) PET/CT with normal findings, Biograph 16 © University of Michigan
B) Cardiac SPECT with normal findings © University of Michigan
C) Apical Hypoperfusion, © Northern California PET Imaging Center
D) Stress-induced lateral perfusion deficit (Upper row: Stress, lower row: rest), MAGNETOM Avanto, © DKD Wiesbaden, Germany
E) Inferior perfusion deficit, visualized by Dual Energy with SOMATOM Definition