Integrated care systems and hospital groups across the country are currently grappling with the challenge of establishing scalable, digitally-enabled community diagnostic centres (CDCs). To find out more about the objectives and challenges involved, we spoke with a number of health system stakeholders who are actively planning local diagnostic provision.
From concept to footfall
In the first phase of CDC development, senior stakeholders made it clear that particular focus should be given to planning for CDCs in a way that will tackle regional health inequalities and drive population health outcomes. It therefore seems logical that with a backlog of examinations mounting, we should seize the opportunity to transform pathways. We should be ambitious and ensure that the COVID-19 pandemic legacy is one that serves to drive radical change.
Whilst the pressures of COVID-19 initially led to a sudden and unplanned drop in imaging demand, many of those we spoke to felt they had restored or were close to pre-COVID activity levels. The issue raised, however, was that the pre-pandemic capacity wasn’t sufficient to deal with the growing patient demand. Add onto this the inherent backlog of examinations generated by the COVID-19 crisis and it becomes clear that overall diagnostic capacity needs to be re-examined. The consensus is that establishing new processes and workflows via the CDC will be critical to delivering the efficiency and capacity needed to transform diagnostic pathways.

A facility fit for purpose
Many have expressed their vision for the CDC as a journey, rather than a project build. This is necessitated by the rapidly changing healthcare needs of the UK population, that vary so greatly depending on location. In the short term, stakeholders expect to witness a gradual shift in patient demand, transferring from settings such as acute hospital A&E and outpatient departments to the CDC. Additional pressures will also need to be accounted for, such as COVID-19 safety. In the mid to long term, as the CDC becomes an established feature of the healthcare landscape, it is likely more demand will be generated for additional services in this setting. With further changes on the horizon, healthcare professionals are clear that adaptability must sit at the core of CDC provision if it is to meet the needs of its local population.
To satisfy local pathway requirements, the sheer number of community diagnostic centre build and design options has rapidly become evident. Popular options discussed have ranged from the establishment of a standard model, featuring defined imaging, pathology and physiological measurement provision to larger models including additional services such as endoscopy, ophthalmology, phlebotomy or training academies established over time. As for the pathways these CDCs must accommodate, cardiac, respiratory and musculoskeletal considerations were most frequently cited, whilst ENT and ophthalmology were mentioned as having a place too.
In terms of CDC location, the picture remains equally complex, with some seeking to adapt existing estate, citing the prohibitive estate costs of establishing and connecting new facilities. Others found, after investigation, that there was simply no suitable space available that met the vision of the CDC. This has made other models, such as the development of new facilities or adopting a hybrid solution built over time, much more attractive options for some. There is one clear consensus that has been voiced to us; whatever the approach, it must be scalable, and tailored to local pathway requirements and the population it serves.

An intelligent workforce
The NHS Long Term Plan set out a workforce implementation plan, while recognising that workforce planning is complex and will always need to be highly adaptive. The spirit of innovation escalated by the pandemic has shown how rapidly the workforce can adapt, and there is a drive to extend this to the CDC to enable its aspirations to reform diagnostic provision. The additional capacity the CDC will provide to tackle diagnostic demand has the entire health system excited, yet one of the most frequently raised concerns is how they will find the workforce to support this. Professor Sir Mike Richards’ Diagnostics: Recovery and Renewal report recognises this challenge, calling for an additional 2000 radiologists and 4000 radiographers.
In the same way that innovation has the ability to transform pathways for the better, many hope that diagnostic reform will act as a catalyst to break down workforce silos and rigid job role definitions. For instance, consideration is being given to enable assistant practitioners to support with routine CT or MR provision, freeing the time of radiographers to focus on supervision and more complex examinations. Similarly, additional capacity requirements for reporting could be alleviated by sharing the imaging skill mix.
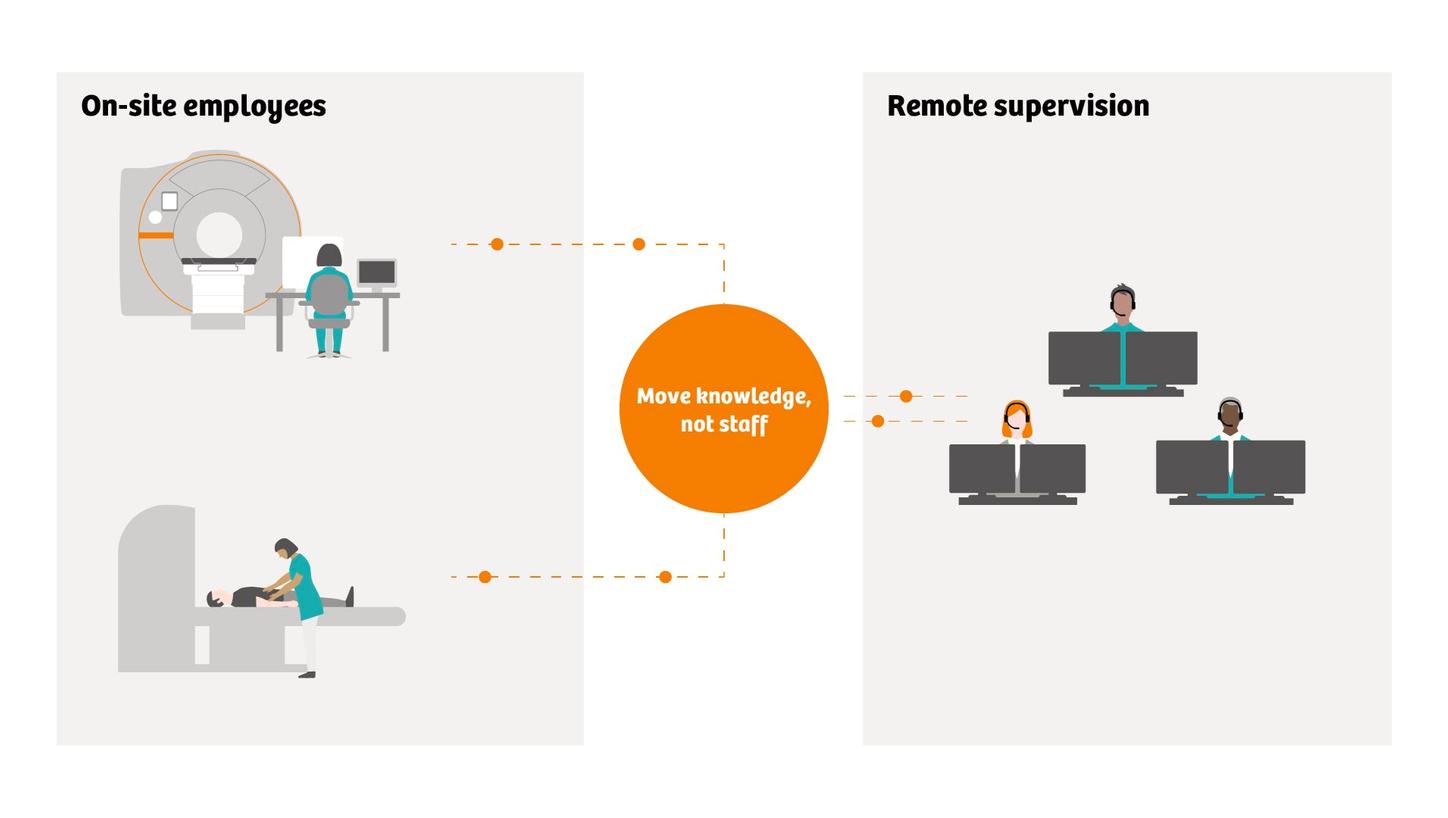
Over the longer term and in the context of sustainability, many view the CDC as a suitable setting to accelerate training and apprenticeship programmes. These could not only upskill the existing workforce, but also act as an attractor of talent from universities and other education settings. This is likely to require a blended approach to workforce education, leveraging virtual platforms. Innovations such as remote scanning assistance, imaging simulators and teacher-led virtual classroom courses are able to supplement traditional on-site clinical applications training. Ultimately, the aspiration for the CDC is one where knowledge is moved, rather than staff, to attract talent, empower the workforce and ensure all examinations are conducted to a high standard.
Digitalisation from the ground up
The need for additional workforce support extends to IT departments. It has been vocalised that additional expertise will be needed, both from within the NHS and external partnerships. In particular, areas such as imaging, echocardiology and endoscopy have been highlighted as those that could benefit from enhanced digitalisation in a community diagnostic centre. At the granular level, this includes technological advancements such as AI to support diagnosis and the planning of care. At the broader level, this encompasses the CDC IT infrastructure at large.
Stakeholders have drawn comparisons with the efforts made by laboratory information systems and pathology networks that successfully scaled network connectivity across the UK at pace. It was agreed that whilst digitalisation was critical to the CDC, it must be supported by optimised pathways and processes.
The complexity of then digitising those pathways was often raised, in terms of data needing to flow between primary care, the CDC and secondary care whilst also building in the flexibility for data to run in both directions, such as for imaging reporting or for reports back to a GP. It was also agreed that whilst RIS and PACS will go some way towards supporting a paperless CDC model, focus needs to be given to enhancing interoperability between different systems. Integration with electronic patient record and intelligent order communications was also raised as a priority, ensuring paper is removed from areas such as patient booking and scheduling tools, and removing issues such as double queries.
Ultimately, an intelligent, fully digitalised workflow infrastructure will be key to helping accelerate diagnosis and ensure right study, right report, right time. Indeed, CDCs present an opportunity to accelerate the generation of diagnostic reports by potentially introducing ‘hot reporting’, the generation of reports whilst a patient is still in the facility. The earlier such reports are generated, the sooner a diagnosis can be delivered and a treatment plan commenced. CDCs offer the potential to accelerate such diagnosis, ideally whilst the patient is still in the facility.
Recovering and renewing diagnostic provision
The pandemic has clearly exacerbated pressures on the NHS and the long-term impact of COVID-19, including the scale of hidden diagnostic demand, remains to be seen. In the many years that Siemens Healthineers has been an advocate of community diagnostics, never has the case for diagnostic reformation and expansion been so clear. There is a real drive within the health system to establish new diagnostic pathways, supported by new ways of thinking around service redesign, build, workforce and digital infrastructure. The system is realistic about the level of complexity involved and continues to work with government to secure the local funding needed to support this. Despite the hurdles to overcome, the community diagnostic centre ultimately represents a significant step towards the panacea of same-day diagnosis, bringing with it the opportunity to increase capacity, reduce waiting times and transform diagnostic provision for the benefit of the patient.

