History
A 56-year-old female patient, suffering from an acute subarachnoid hemorrhage, was admitted to the emergency department. The patient had had a ruptured cerebral aneurysm, which had been surgically clipped seven years ago and had been experiencing refractory hypertension throughout the past seven years. She reported a previous “congenital cardiovascular malformation”, however, could not provide any details. A CT angiography (CTA) of the chest and abdomen was requested for further assessment.
Diagnosis
CTA images showed a severe coarctation of the aorta, immediately distal to the dilated left subclavian artery (LSA). Abundant collaterals, formed by bilateral enlarged internal thoracic arteries, as well as the superior and inferior epigastric arteries, were seen. Dilated superior thoracic arteries, lateral thoracic arteries, subscapular arteries and posterior collateral intercostal arteries to the post-coarctation descending thoracic aorta (DTA) were also visualized bilaterally. There were no signs of a patent ductus arteriosus or other cardiac abnormalities. The patient was referred to a higher-level hospital for further treatment.
Fig. 1: Two cVRT images (Figs. 1a & 1c ) and a MIP image (Fig. 1b) show a severe coarctation of the aorta (arrows) immediately distal to a dilated LSA. Dilated branches of bilateral subclavian arteries and post-coarctation DTA are clearly shown as well (Fig. 1a, 1c & 1d).
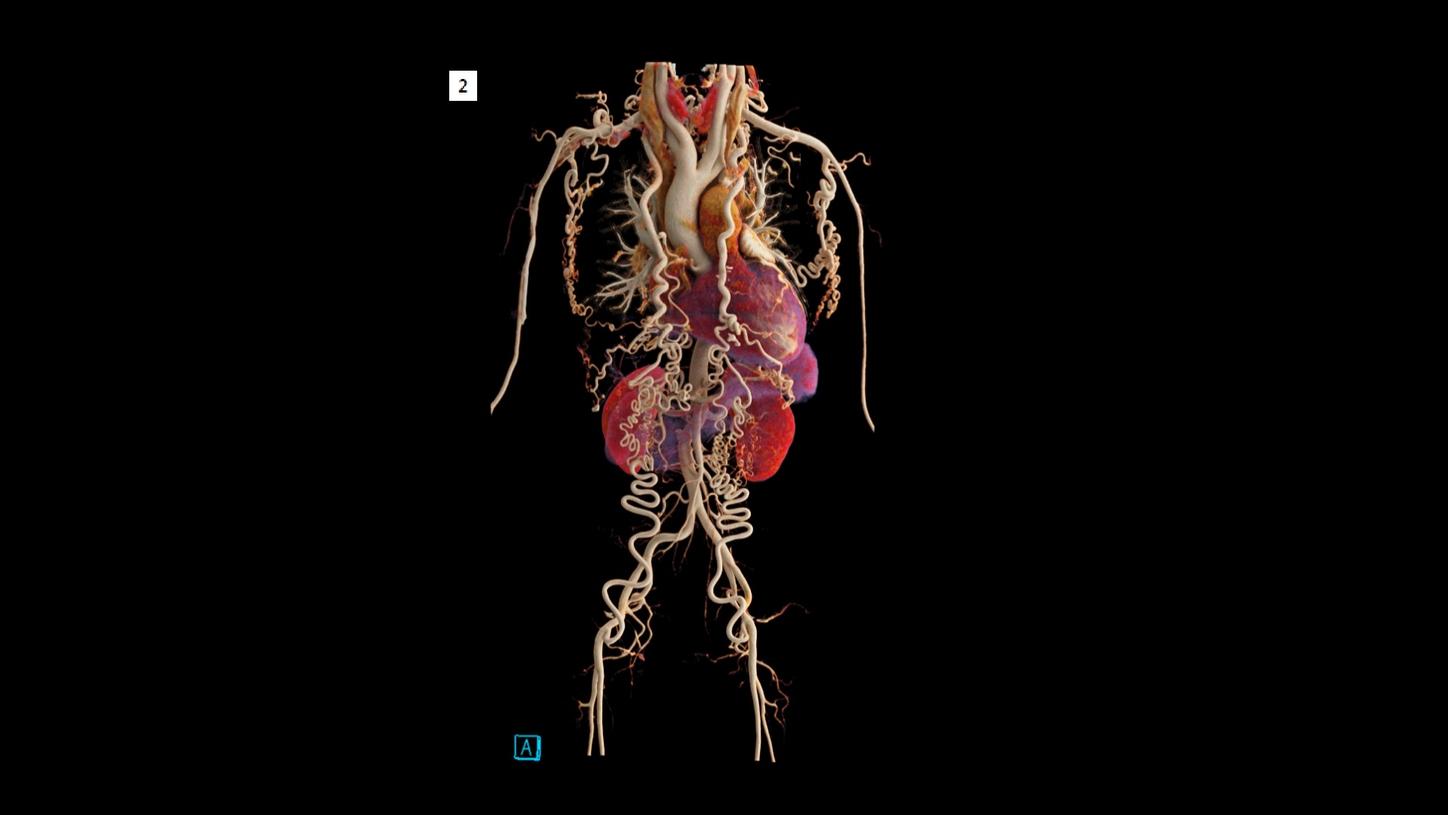
Fig. 2: A cVRT image shows an overview with abundant collaterals, formed by bilateral enlarged internal thoracic arteries, superior and inferior epigastric arteries, as well as dilated branches of bilateral subclavian arteries.
Comments
Coarctation of the aorta is a congenital malformation and is commonly represented by a localized constriction of the aortic arch or proximal DTA. It is a typical disease of childhood and early adulthood. If left unrepaired, serious complications such as hypertension, cerebrovascular hemorrhages, aortic valve destruction, premature coronary artery disease and aortic aneurysm or dissection, may occur resulting in death at an average age of 33 years. [1] Surgical or interventional repair can be effectively carried out and devised accurately with morphological information concerning the location, degree and length of narrowing, presence of collateral circulation, relationship to the LSA and associated cardiovascular abnormalities. CTA with multiplanar and three-dimensional techniques is the noninvasive method of choice for the assessment of these parameters, [2] as well as for post-repair follow-up. In this case, a 70 kV setting is applied to enhance the contrast-to-noise ratio, resulting in a reduction of the radiation dose as well as in the amount of contrast agent needed. For three-dimensional image demonstration, cinematic volume rendering technique (cVRT) is used to provide a lifelike visualization, facilitating the communication between physicians and with the patient.
Examination Protocol