By Mario Jreige, MD; Marie Nicod Lalonde, MD; Niklaus Schaefer, MD; and John O. Prior, PhD, MD
Data courtesy of Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland
History
A 62-year-old man with primary prostate cancer, diagnosed on clinical examination and transrectal ultrasound, underwent 68Ga PSMA PET/CT for initial staging. The PET/CT study was performed on Biograph Vision™. 68Ga PSMA (2.8 mCi, 105 MBq) was injected intravenously and a PET/CT study was performed after 1 hour and 5 minutes. An initial whole-body CT (100 kV, 104 eff mAs, 64 x 0.6 mm collimation) was performed, followed by a continuous bed motion (FlowMotion™ technology) PET acquisition with a constant table speed of 1.0 mm/sec. The PET study was reconstructed at 440 x 440 matrix using time of flight (ToF) and point spread function (PSF).
Findings
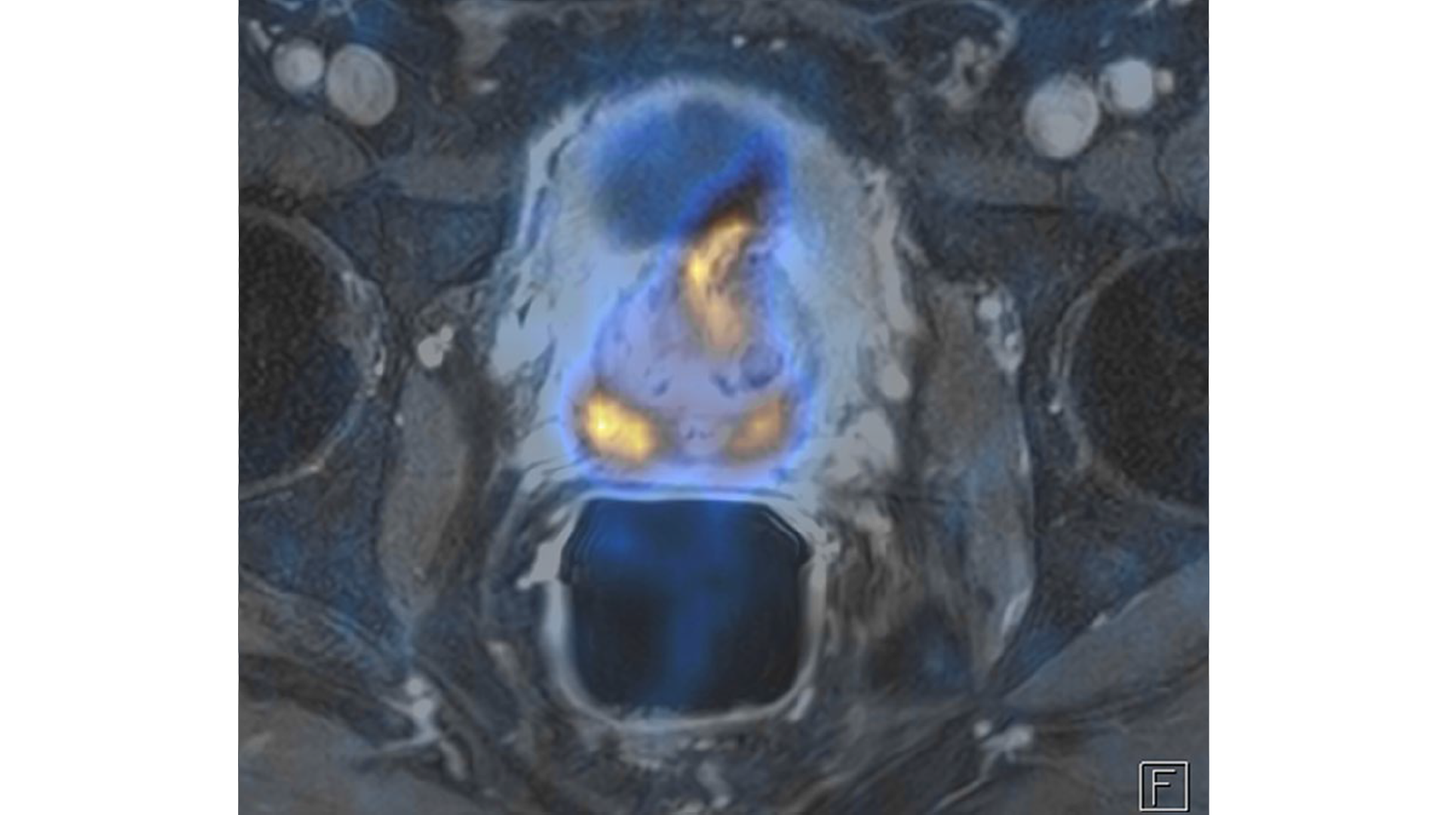
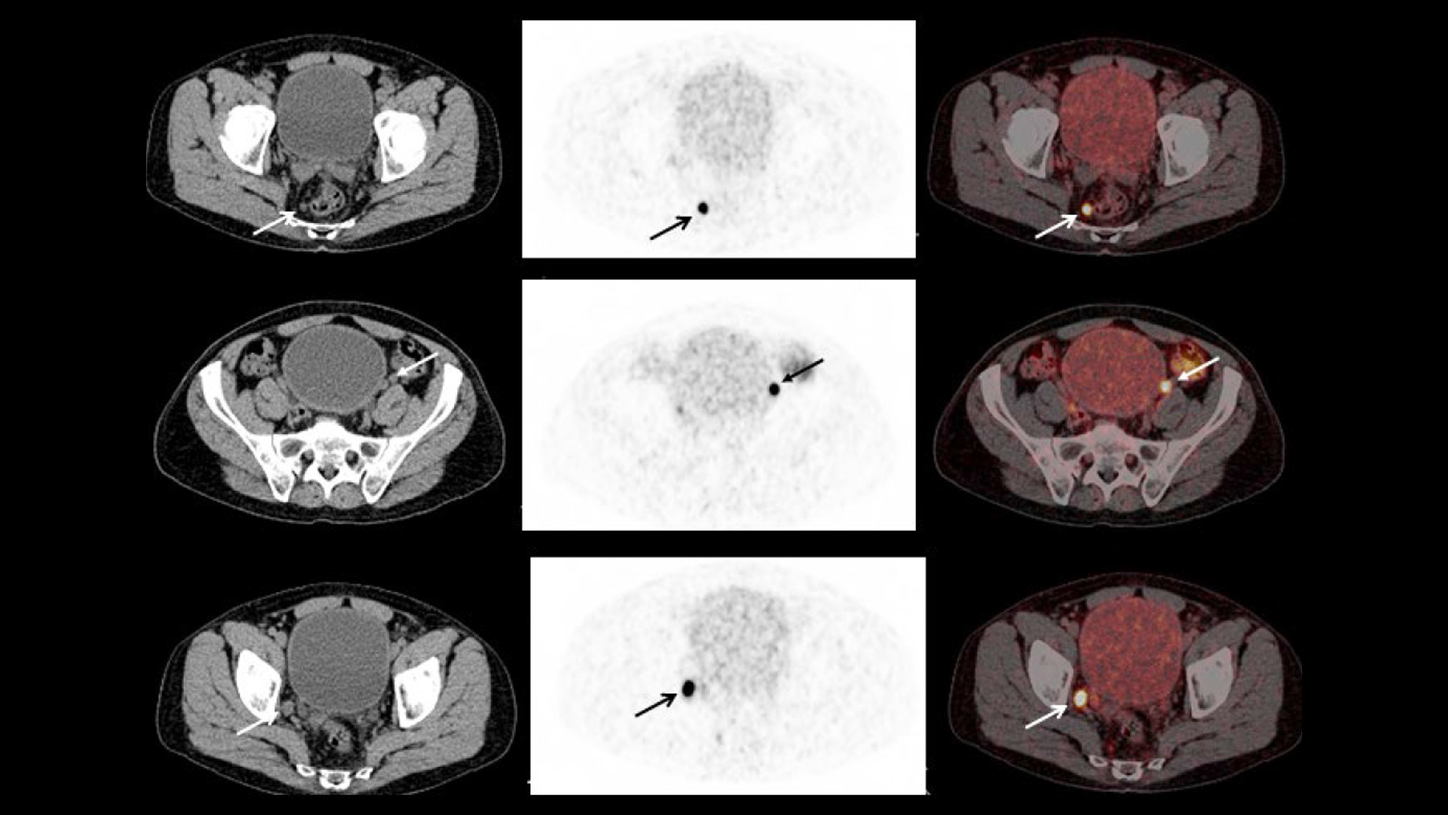
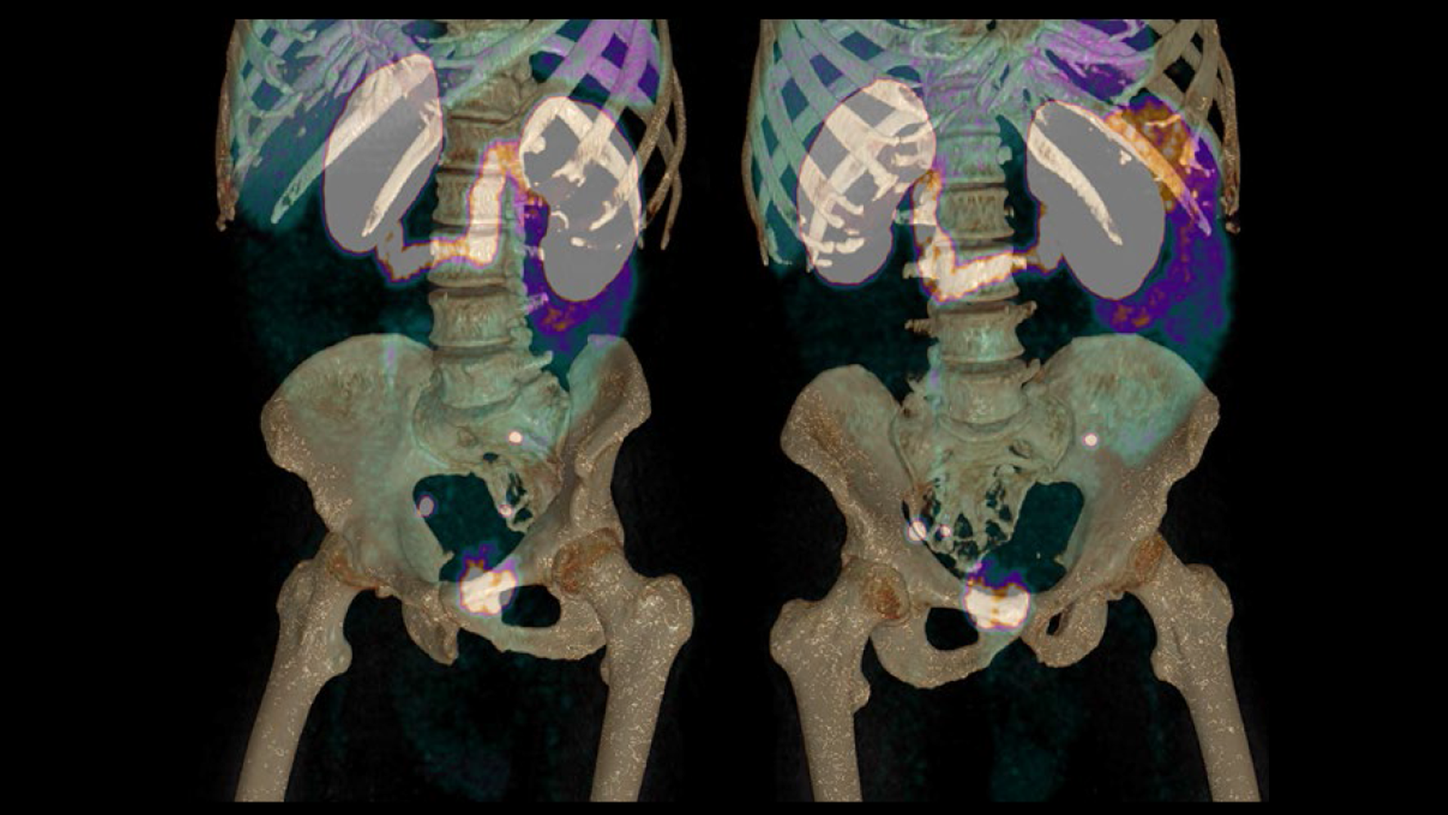
68Ga PSMA PET/CT (Figures 1 to 6) shows primary prostate cancer involving the majority of the enlarged prostate gland measuring nearly 3 cm in all dimensions with invasion into the bladder neck and external urinary sphincter (T4), with resulting bladder outflow obstruction. The PET/CT also revealed three highly tracer-avid pelvic lymph node metastases in the right meso-rectal, right external iliac and left common iliac nodes. No distant metastases were visualized.
Bladder invasion by primary tumor and the presence of pelvic nodal metastases puts the patient in stage IV. The primary prostatic tumor showed high intensity of 68Ga PSMA uptake with a SUVmax of 37.3. The pelvic nodal metastases were also highly tracer-avid with the SUVmax ranging from 36 to 56. The meso-rectal and left common iliac nodes measured 8-9 mm in diameter but were intensely tracer-avid with high lesion contrast, with the highest SUVmax being in the left common iliac node. Physiological uptake of 68Ga PSMA in the salivary glands, liver, kidney, and intestines were within normal limits.
PET, CT, and fused images at the level of the prostate, from Biograph Vision, show high uptake of 68Ga PSMA in the primary prostate tumor with extension into the adjacent bladder wall.
Comments
The presence of lymph node metastases in primary prostate cancer patients is associated with adverse prognosis. The presence of bladder neck invasion from a primary prostate tumor along with multiple pelvic lymph node metastases in this patient put him in stage IV, which requires systemic therapy. Therapy options in such patients include radical prostatectomy with pelvic lymphadenectomy or radiotherapy along with neoadjuvant or concurrent anti-androgen therapy (ADT). Detection of lymph node and distant metastases is the most critical factor in accurate staging of primary prostate cancer, which influences further therapy choices. The detection rate of pelvic lymph nodal metastases and distant metastases at initial diagnosis is around 20% and 10% respectively and is impacted by serum prostate-specific antigen (PSA) levels.1 The effectiveness of definitive radiation therapy depends on accurate definition of extent of direct extraprostatic extension and detection of pelvic lymph node metastases in order to ensure adequate dose delivery to target volumes. 68Ga PSMA PET/CT has been shown to improve the success rate of radiation therapy in primary prostate cancer by identifying patients with occult metastases and thereby modifying target volume delineations and dose plans in order to adequately cover local disease.2
Radiation target volumes that were created using only CT were compared to 68Ga PSMA positive lesions in a study involving 73 patients with high risk primary prostate cancer (PSA>10 ng/ml) to determine whether PSMA-positive lesions were localized inside or outside of irradiated volumes.2 Twenty-five out of 73 patients (34%) showed 68Ga PSMA-positive lymph node metastases, while only 7 of 73 (9.5%) showed enlarged nodes suspicious for metastases on CT. 16.5% of patients had at least one PSMA-positive lesion not covered by target volume based on CT. 5.5% of patients had at least one centimeter of primary prostate tumor not covered by CT-based radiation target volume. In these patients, PET/CT had a major impact on radiation therapy planning leading to a change in the target volume. The majority of PSMA-positive lymph nodes not covered by CT-based plan were in perirectal or common iliac nodal groups. The median size of PSMA-positive lymph nodes missed on the CT was 6 mm. In all patients with nodal lesions or periprostatic extensions identified by PSMA PET/CT, radiation plans were modified with dose escalation to PSMA-avid lesions. Similar impact on the therapy plan is expected in this patient to manage the infiltration of bladder neck by primary tumor as well as lymph nodal metastases. The meso-rectal and left common iliac nodes were 8 mm in diameter but highly PSMA-avid and the radiation fields need to include these nodes along with the right external iliac nodal metastases with dose escalation to PSMA positive lesions.
Although the avidity of prostatic malignant cells for PSMA is the key driver for 68Ga PSMA PET/CT due to its ability to accurately define a primary tumor and peri-prostatic extensions and detect small lymph node metastases, PET/CT image quality, resolution, and lesion contrast is of utmost importance in order to ensure the highest sensitivity of the study. Technological improvements in PET/CT such as incorporation of SIPM technology for improved ToF performance for improved lesion detectability may potentially further improve sensitivity of PET/CT for detection of nodal and distant metastases with direct impact in staging and management. In this context, Biograph Vision with a 214 picosecond ToF timing resolution and 3.2 mm crystal size is able to provide very high lesion contrast and high resolution imaging that sharply defines primary prostate tumor and the bladder neck invasion as well as tracer avid lymph node metastases, the smallest of which in this case was 8 mm in diameter. The reconstruction matrix for the whole-body PET study was 440 x 440, which reflects the high resolution of Biograph Vision enabled by the small 3.2 x 3.2 mm crystal size. Smaller crystal size enables higher resolution acquisition, which reduces partial volume effects that often impact the definition of small lesions and improves quantitative accuracy. The high SUVmax of the small nodal metastases as small as 8 mm as in the left common iliac node is testament to the high lesion contrast generated by 214 picosecond ToF timing resolution as well as reduced partial volume effects enabled by high resolution imaging on Biograph Vision.
Conclusion
High lesion contrast and resolution enabled by Biograph Vision was instrumental in sharp definition of invasion of bladder neck by aggressive primary prostate cancer along with multiple, small pelvic lymph node metastases by 68Ga PSMA PET/CT.