One of just four hospitals in the Walloon Brabant province, Clinique St Pierre Ottignies plays a pivotal role in innovating to fit a rapidly changing medical landscape. The hospital is aware of its responsibility to its patients first and foremost, but also to its staff who strive every day to push the quality of care to the highest possible level.
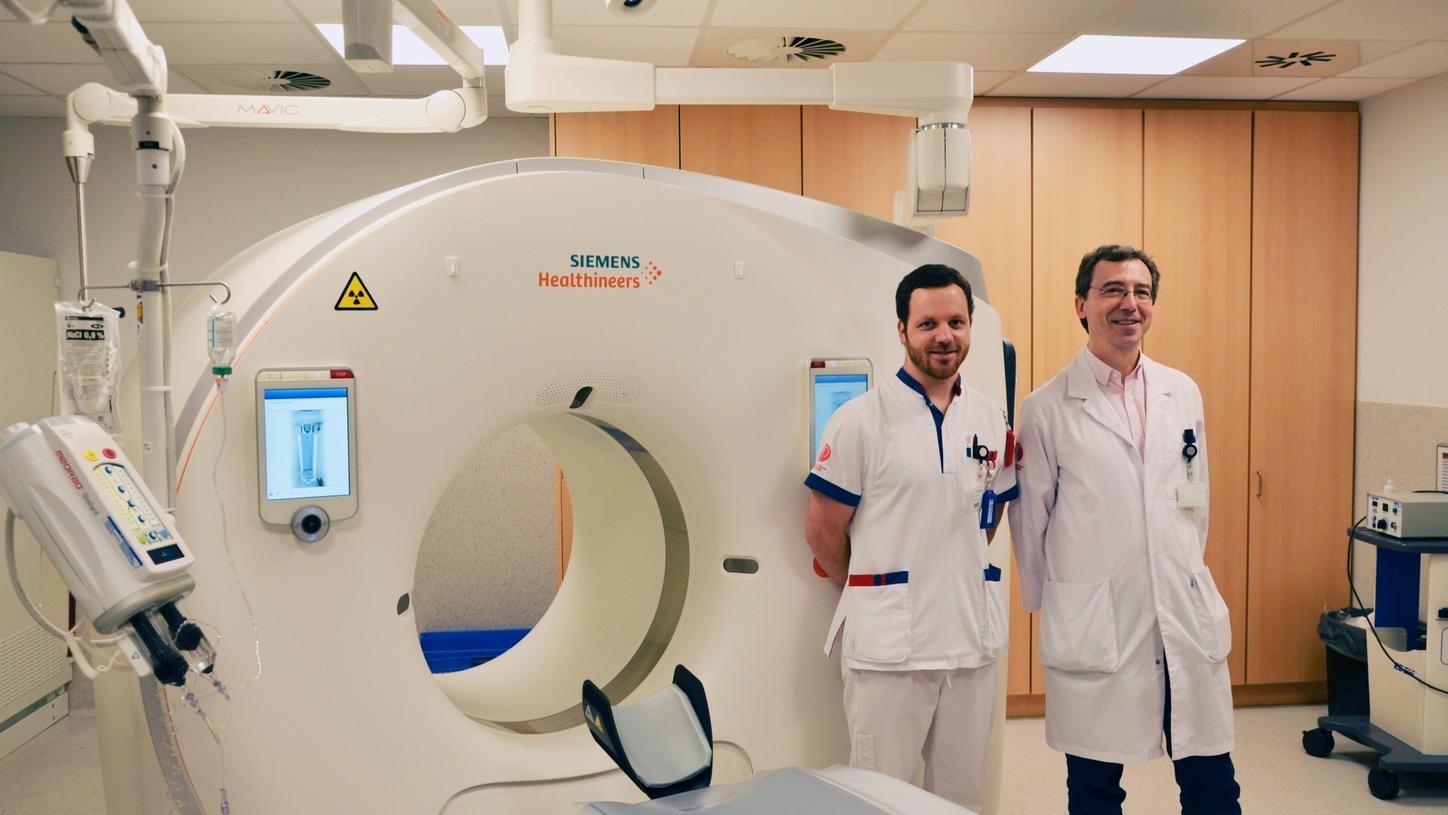
At the radiology department, typically the backbone of a hospital, these values were central in their decision to replace their former CT scanner with a SOMATOM Drive. Radiologist Emmanuel Agneessens, MD, and Michael Vandamme, technologist, were eager to share their initial experiences with their new system and talk about the clinical benefits.
The scanner allows us to work with more confidence, both on a purely practical as well as on a diagnostic level. We can explore new clinical fields that weren’t open to us before.
Could you elaborate a bit more on what you mean by exploring new clinical fields?

Agneessens: “Well, I think one of the major benefits of this system is its Dual Energy capabilities. For instance, in pulmonary angiography, I strongly believe that DE scans (utilizing Lung PBV) should be performed as standard. It lets me see things that I might have overlooked before, not least pulmonary emboli, where conventional single energy scans just don’t give you the detail you need. That’s what I mean by bringing more confidence to our work.
Also, in an oncological setting, the possibility of having iodine maps and the opportunity to play around with different kV values, is a tremendous step forward. Our goal is to refer every single oncology patient for a CT scan. We’re even looking at the possibility of shifting certain examination types from other imaging modalities (i.e. Nuclear Medicine) to our new system.
Furthermore, I am convinced that DE scans can take our emergency care to a next level. It would have advantages in head scans, for example, to support in visualization of hemorrhages or additionally for abdominal pathologies, as in evaluations of the digestive system. Ideally, we’d use the CT scanner for all our emergency cases, 24/7. My personal goal is to have this set up by March 2019.”
Vandamme: “One of the reasons why we want this system to be our dedicated emergency CT scanner is the impressive acquisition speed. This is particularly useful in imaging challenging cases such as obese patients. The fact that we can combine iMAR (iterative metal artifact reduction) with DE truly adds value here for our patients and their clinical outcomes.”
Agneessens: “By the way, the interest in scanning with Dual Energy goes beyond the radiology department. Even today, we are getting requests from our colleagues in the orthopedics department to perform their scans with DE as well as from our colleagues in the cardiovascular department.”
Apart from that, do you see other advantages, for instance directly related to the patient?

Vandamme: “We now routinely perform virtual noncontrast scans, which means less time for the patient in the scanner room. And by using DE, we avoid the radiation dose of a true noncontrast scan, of course. To save dose, we also apply the Tin Filter for all our sinus, colon, and thorax exams. Even in our Calcium Scoring protocol, we use the Tin Filter (Sn100 kV) together with the Flash scan. This can lead to unprecedented dose levels in our cardiovascular examinations.
The scanner automatically selects the appropriate low kV value (70, 80, and 90 kV) without any loss in image quality. This of course has a positive impact on the radiation dose, too. The number of scans we perform at 120 kV or higher has decreased dramatically.”
Agneessens: “It’s not only radiation dose, however. We’re also able to significantly decrease the amount of contrast media (volume and/or concentration) we administer to our patients through these low kV values. This enables us to potentially scan patients we wouldn’t have been able to before.”
“We use the Tin Filter (Sn100 kV) together with the Flash scan. This can lead to unprecedented dose levels in our cardiovascular examinations.”
“Regardless of who is operating the system, the patient is always placed at the isocenter of the gantry.”