The second Executive Summit panel begins with the premise that “where care happens matters” and that this substantially impacts patient health. Three significant trends are driving the healthcare industry toward the outpatient setting. Finance is first on the list. Governments, payers, and healthcare systems are attempting to shift healthcare facilities to lower-cost areas. The second is associated with safer therapies that, because of advances in technology and healthcare, may be moved out of the acute inpatient setting and into locations closer to home, places where a patient can feel cared for. As for the third—on the rise since at least the advent of COVID-19—is that patients demand more control over their therapy, both in terms of where and how it is administered. The panelists in this session believe that the location of healthcare delivery and the promotion of health to prevent illness are of utmost importance in achieving the goals of increasing efficiency while decreasing costs.
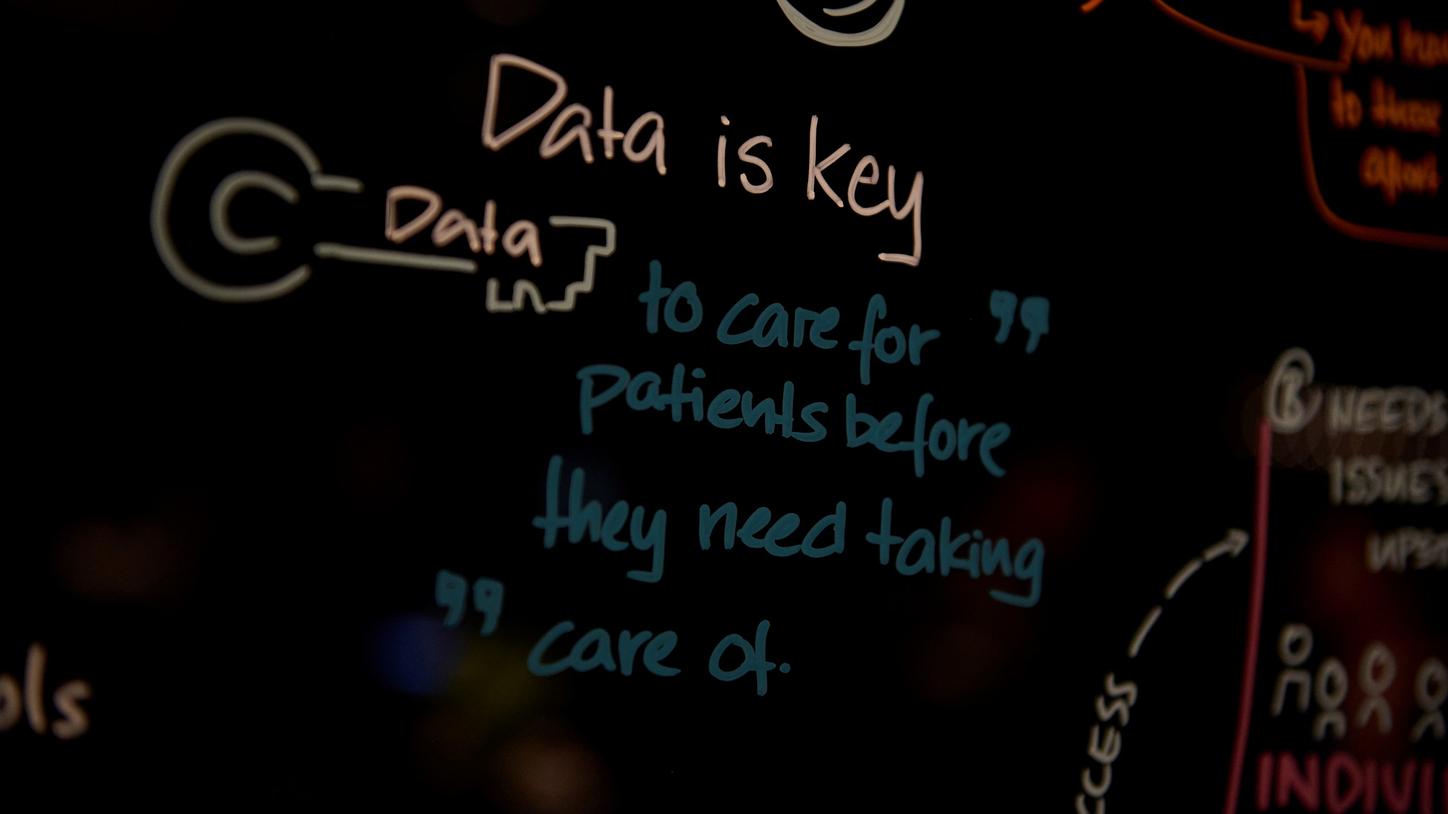
Patient data can be the key to deliver predictive, proactive, and preventive care.
Using artificial intelligence and data in a way that appears almost science fiction, a leading healthcare institution in Israel is making a difference in providing the proper treatment at the right time. There is the need of a paradigm shift to solve the ever-present issue of rising population and demand, while lacking the healthcare professionals to increase care delivery. Israel’s most prominent healthcare payer-provider is mainly oriented on primary care, and aims to revolutionize healthcare by using 25 years’ worth of patient data to deliver predictive, proactive, and preventive care. “You should come to the patient when they look healthy,” it was stressed.
The healthcare institution’s approach to the distribution of yearly flu vaccines was used as an example; it is organized by the risk of winter morbidity and influenza complications, and ensures that everyone at risk receives the dose. In addition, the Israeli healthcare institution is starting to leverage the data acquired over the years to put into reality the concept of digital twins, which they fully exploit during COVID-19 to simulate clinical trials using retrospective data. With the use of highly in-depth digital twin-matching technologies, they were able to demonstrate what works and what doesn't. This proved the effectiveness of such initiatives in reducing hospitalization rates by 43% and their cost-effectiveness.
To enable physicians to choose the correct patients to be treated at the right time, they developed a system for picking the most appropriate patients for treatment. In summary, the most important factors for success from the Israeli healthcare institution’s point of view are integration “by design,” investment in primary and at-home care; incentives that are properly matched; information technology infrastructure; and innovation in practice. This unique approach was stress-tested during COVID-19 when their prediction algorithms were utilized to alert high-risk patients to seek treatment at home rather than in the hospital.
When asked about how to best engage physicians in the paradigm change, the panel emphasized the importance of adapting to their workflow rather than imposing new ideas onto them. Physicians should also be trained on how to utilize the new innovative process. It is also essential to ensure they strongly desire to participate in the proposal. Mark O’Halla, President and CEO of Prisma Health, chimed in, adding, “As long as our medical group recognized the benefits that were going to accrue to them by making these changes, they were quite supportive and really helped drive the process.”

Robert Möller shares how Helios Kliniken is challenging the status quo of the German healthcare system by adopting digitalization and portability.
The absence of incentives to build a common platform to disseminate data was cited by all panelists when questioned about the obstacles that hinder the route toward a widespread Israel model. However, difficulties may vary across countries owing to varying cultural constraints. Robert Möller, CEO of Helios Kliniken, depicted a vivid picture of the German healthcare system, portraying it as a complex and costly system overly focused on preserving the status quo rather than finding effective solutions to medical issues. Möller deduced the causes, one of which is an excessively traditional society infused with a dread of the unfamiliar. Möller added, “decision-makers in regional and federal politics are most afraid of the risks involved in any upcoming election.” Twenty years after the last substantial reform of the inpatient hospital system, “what can we do today?” Möller asked.
He believes that the first step is to overcome the belief that the strength of hospitals is based on the hotel business rather than on a high degree of knowledge that allows the prompt availability of methodical competence. As part of this shift, Helios Kliniken is implementing a new approach to healthcare called “Care for you to be,” or CUBE. The purpose of the CUBE is to fill the gap left by the absence of general practitioners and bring medicine to the patients. It combines several different diagnostic tools into a single, portable package, allowing it to be set up anywhere from a retail store to a remote location. Basic medical treatment and diagnosis will be available at the CUBE, a physical space overseen digitally by healthcare experts connected to the Helios system. However, “it’ll only work, when we manage to rapidly update in the field of digitalization without losing sight of those patients outside hospitals […] we now have drawn up a strategy of digitalization that is clear, comprehensible, ambitious, cutting-edge, and feasible,” Möller ended.

Mark O'Halla explains how Prisma Health reduced costs significantly by increasing the number of mobile care clinics while attempting to eliminate barriers to home-based care.
The fact that 94% of patients are satisfied with Prisma’s healthcare system proves that such a framework is viable. Prisma Health covers two-thirds of the geographically diverse state of South Carolina. The organization is actively pursuing a transition from inpatient hospital care to outpatient, home-based care to bring care to rural and remote areas. COVID-19, according to O’Halla, pushed them to “look at the universe in dramatically different ways.” They increased the number of mobile care clinics while attempting to eliminate barriers to care to treat seriously ill patients at home, dropping costs significantly by 13%.
O’Halla’s vision is to become more than just a care provider, noting that “if you are just a care provider, you are at the end of the payment stream, and you become a commodity.” Both Prisma and its client companies realize cost savings since they deal with self-insured businesses that pay for any outlier claims themselves.

Jeremy Fotheringham shares how SSM Health is in the path from rescue to preventive care and overall health by partnering with mayors, health departments, and legislative plans.
SSM Health Saint Louis is another reality in the path from sick to preventive care and overall health and wellness. Regional President of SSM Health Saint Louis, Jeremy Fotheringham, indicated that they embarked on this journey because healthcare costs are excessively high. Yet, life expectancy in the United States is one of the lowest across mature markets, mainly due to obesity, which leads to the highest rates of chronic illnesses. Fotheringham elaborated on SSM Health’s need to address therapy, health, and well-being as a whole. When it comes to affecting health, wellness, and bettering communities, “we need to step further upstream, both at the individual and community level, by creating policy and practices,” Fotheringham said.
By looking at the factors that impact an individual’s health, they determined that only 20% comes from actual healthcare, such as access and quality of care; 80% comes from the individual behaviors, their immediate surroundings, and socioeconomic status. This means that the zip code heavily influences a person’s health. Shockingly, only 3% of healthcare dollars spending goes toward the variables that lead to that 80%, whereas 97% goes into healthcare services. Focusing on policies and practices will “bend the cost curve,” Fotheringham stated. The 18-year difference in life expectancy between the north and south of Saint Louis served as an example. The difference coincides strongly with the quantity and density of supermarkets, making it difficult for patients to adhere to a healthy and low-calorie diet to combat obesity.
The same holds true for healthcare clinics and educational institutions, and “because you don’t have access to good food, the entire healthcare system spends an additional $155 billion annually,” Fotheringham remarked. SSM Health developed the Vibrance approach, a data and clinically driven and patient-centric style of care, to kick-start its new way of thinking. The new strategy aims to influence health equality by partnering with mayors, health departments, and legislative plans to develop upstream systems of care and incentives. Fotheringham concluded, “there is a great deal of trust to rebuild, and we have the opportunity to do it.”

Further Reading: Insights Series
The Siemens Healthineers Insights Series is our preeminent thought leadership platform—carefully researched and professionally written papers drawing on the knowledge and experience of some of the world’s most respected healthcare leaders and innovators. The Series explores emerging issues and offers ideas, analysis, and practical advice on how to deliver high-value care.





