Home
Perspectives
- Harnessing digital technology for laboratory diagnostics

Harnessing digital technology for laboratory diagnostics
The future clinical laboratory is the stuff of science fiction. Services like touchless inventory control and auto-validation of testing are gradually becoming commoditized, with built-in quality control features to ensure high standards.
With these innovations, lab staff now have more time to focus on the growing range and complexity of testing options, and physicians will seek their counsel regularly in coming years.
IT meets patient needs and laboratory goals
If a genie were to offer three wishes to laboratory administrators around the world, their responses would be similar, regardless of their hospital or lab facility.
A first wish would be for better patient-centric care and outcomes. Another might be for increased staff satisfaction, given the shortage of qualified lab technicians in many countries. The third would be for improved lab efficiency – faster turnaround time (TAT), reduced paperwork (or none at all), fewer errors, more effective employee training, better inventory management, improved quality control despite increased test volumes, and detailed traceability logs. All three wishes would be granted with no increase in staff or operating costs, and, if the results saved money, so much the better.
Today’s digital laboratories are fulfilling these wishes. Digital laboratory solutions can harness the power of information technology to improve operations in ways not imagined when the first laboratory information system (LIS) was introduced in the 1980s. The potential of digital solutions to improve laboratory workflows is increasing because the world is becoming more connected. The Internet of Things (IoT) is a reality today, interconnecting and allowing smart devices to communicate with each other. At the same time, enhanced computing power is transforming this data into better service for patients, staff, and hospitals.
“The digital lab has really taken off in the last two years,” observes Alejandro Mora, Head of Diagnostics IT Ecosystem – Europe Middle East & Africa at Siemens Healthineers in Frankfurt, Germany. “Now IT can do a lot more with less.” He points out that digital labs can both free specialists for the work they do best, and use captured information to save money and identify future improvements, simply by organizing the volumes of data that flow through a laboratory daily, supervising process flows, managing point of care (POC) devices, and handling inventory automatically.
Inventory control
For example, a single laboratory with 48 employees, including 42 lab technicians, services the sprawling Universitätsklinikum (University Hospital) complex of Essen, Germany, with its 70,000 inpatients, 171,000 outpatients, and 7.8 million lab tests annually. The lab’s chief chemist Bernd Wagner, PhD, relies on digital solutions across the board, including inventory management.
Traditional inventory functions had been manually executed; they were inconsistent and prone to error. Automated inventory control has made possible a huge improvement in staff time allocation, increasing the quality, traceability, storage, and accuracy of orders, and decreasing waste. “Delivery is within 24 hours,” says Wagner, “and inventory handling is 35 percent faster so our employees can focus on lab work.”
The digital lab easily handles other rote chores like labeling tubes, validating blood tests, checking patient records, generating basic reports, keeping track of staff training schedules, and periodically testing equipment for accuracy.

POCT management
With 70 sites and 3,000 operators of point-of-care devices, St. James Hospital in Dublin faces ongoing challenges for the training and management of staff and the assured quality, accuracy, and security of information. Thus, its ISO 15189/22870 certification is a point of pride for the largest teaching hospital in Ireland.
Felicity Dempsey, who was the hospital’s POCT manager for more than a decade (she is currently a consultant to St. James), found the solution in digitalization. She wanted a system of fully verified POCT devices that enabled different levels of access depending on the operator – doctor, nurse, or other specialized staff. She wanted the system to automatically set in motion the recertification of operators at specified intervals, and fixed objective criteria for this process. Training is important because, she explains, “Our staff have different skill sets and levels of interest.” Normal recertification is every two years, but doctors in Ireland may rotate among hospitals every six months, so flexibility was needed.

The system needed to be adaptable in other ways. It had to be compatible with HIS and LIS. It had to be able to integrate the hospital’s 300 POC devices, so there are 190 different drivers available for easy device integration. Quality needed to be consistent across all sites, with impeccable paperless trails to ease ISO reaccreditation. Over the last five years St. James has been accredited with no non- conformance found.
Corollary benefits include a 33 percent reduction in consumables (by monitoring reagent usage). Troubleshooting time was cut in half, to three hours a week. The staff spends less time on day-to-day maintenance and more time on clinical audits, with additional improvements in patient outcomes. Only two people manage the entire POC operation. “This would have been impossible without digitalization,” observes Dempsey.

Data management
Swedish Covenant Hospital in Chicago, Illinois, is a mid-sized city hospital with 312 beds and a few peculiarities: 40 languages are spoken by its staff and they handle more than 285,000 outpatient visits a year. Its laboratory of 65 fulltime-equivalent (FTE) employees does 1,400,000 tests annually.
Susan Dawson, laboratory administrative director, wanted to increase efficiency, ensure topnotch results for patients, eliminate paper, and improve quality of life for her staff. She introduced data management digitalization in 2002 and has been enriching and fine-tuning the system ever since. Today the system is paperless from the physician’s order to labeling, processing, analysis, review, verification, and reported results. No errors occur from misreading a doctor’s order (physicians’ handwriting is notoriously illegible), a label, or a bedside binder because all is digital.
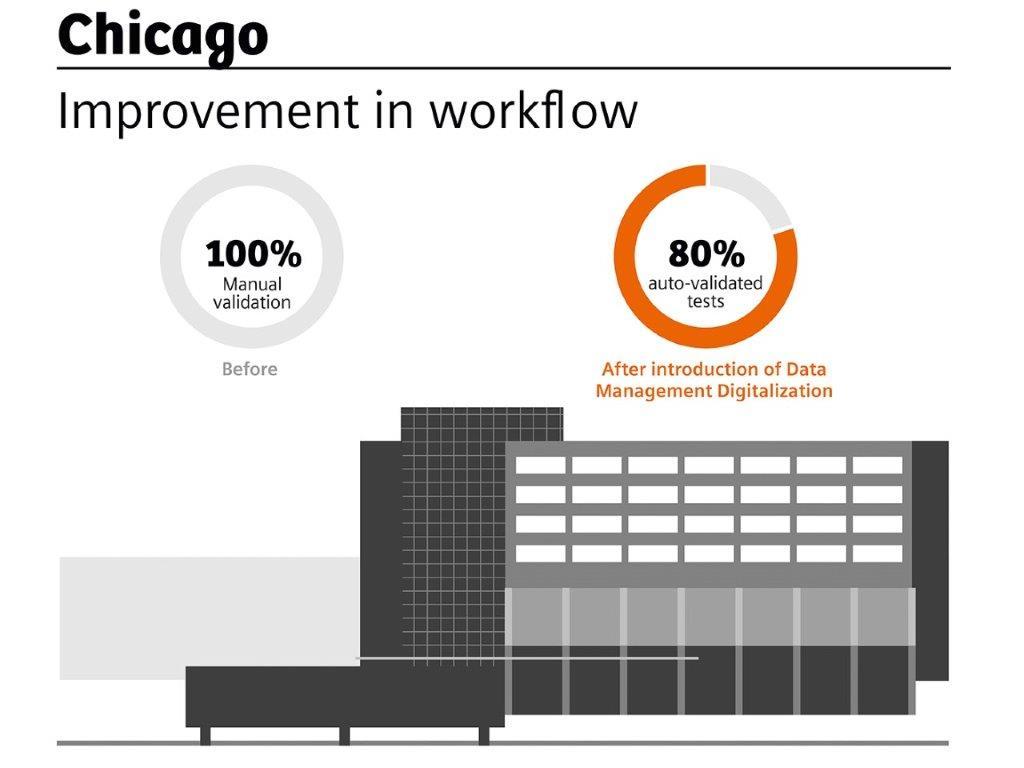
Auto-validation of testing has resulted in a major improvement in workflow. Technicians focus only on tests that fall outside of an established range, while the 60–80 percent of tests that can be auto validated are processed automatically. Technicians love this feature because it saves time, relieves boredom, and reduces errors.
Dawson admits that some of her staff resisted when the system was first proposed. She won them over by investing them in the project: What information did they need? How should it be visualized? How could color-coding be used to improve comprehension? Because the system is flexible, modifications have been easy to implement, and improvements continue to this day. Quality is up, manual labor is down, and employees are more energized. “An empowered staff equals positive results,” she notes.

Flexibility and the future
Flexibility is key to a well-designed digital solution for many reasons:
- A digital solution may consist of a number of suppliers; flexibility is needed to integrate them effectively.
- A hospital may merge into a larger network, so its digital solutions need to be adaptable.
- Technology continues to evolve, so a hospital may want to add new features periodically.
Tomorrow’s digital lab is already taking shape, and AI (artificial intelligence) will play a major role in its development. There is no other way to handle the volumes of Big Data being generated, and the healthcare industry is just beginning to grasp their significance, claims Gian Franco Gensini, MD, of the Società Italiana di Telemedicina (Italian Society of Telemedicine). In the future, he suggests, such information will be used to identify case patterns, develop instructional materials, support decisions, and predict outcomes, all with complete traceability.
Mora of Siemens Healthineers notes that laboratories and hospitals are obliged to store data for determined periods, so it makes sense to leverage this information for operational improvements. Already pilot programs exist to facilitate risk assessment for specific diseases, support diagnoses, and suggest customized therapy options. The examination of millions of cases and massive amounts of data helps personalize treatment, while the doctor-patient relationship remains inviolate.
That is the essence of healthcare technology – data-driven systems to support people, physicians and patients, at the core. No genies needed.
Related Links
- The statements by Siemens Healthineers customers described herein are based on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist (e.g., hospital size, case mix, level of IT adoption) there can be no guarantee that other customers will achieve the same results.











