Prostate cancer: Facts, diagnosis, and treatment
Facts
Prostate cancer remains a uniquely challenging and complex illness, with significant complications and unpredictable treatment outcomes. Despite the advances made in recent years, it remains the fifth leading cause of death worldwide and the second most frequent cancer diagnosis in men [1].



Diagnosis and Staging
What if a doctor suspects a patient might have prostate cancer?
During diagnosis, a patient will be asked about any symptoms as described above and about possible risk factors including his family history. In case of any suspicion, the doctor might order some tests.
Treatment
Catching prostate cancer early makes it highly curable.
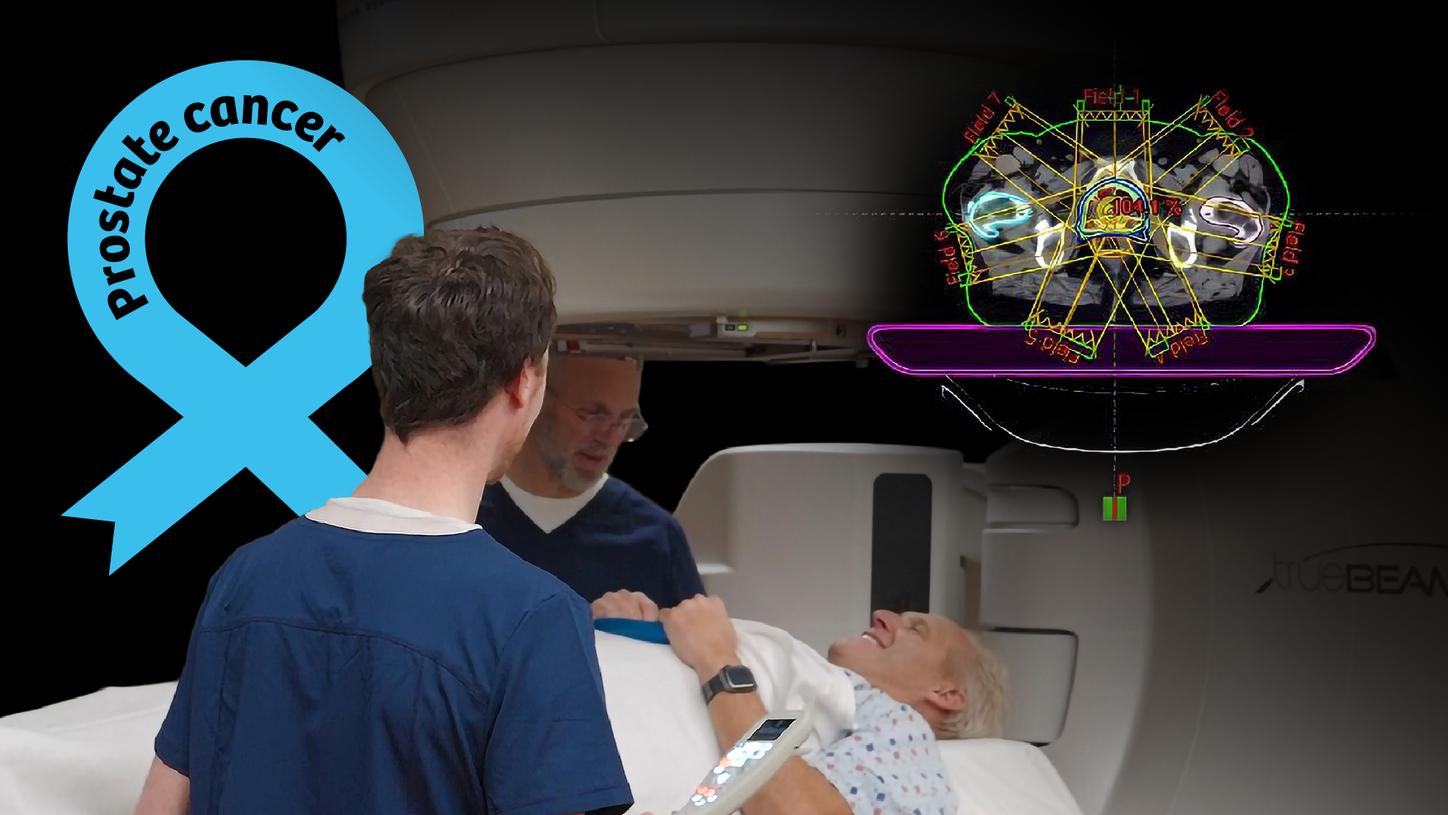
VARIAN EclipseTM IMRT (Intensity Modulated Radiotherapy) plan for a prostate cancer patient.1
Most often men are diagnosed with localized disease, but 10–20 percent are diagnosed with metastatic disease and of those battling localized disease, 20–30 percent will develop metastases [25].
70 percent of those diagnosed with advanced prostate cancer and 90 percent of men who succumb to the disease have bone metastases [25].
[3] https://doi.org/10.4103/tcmj.tcmj_20_17
[4] https://seer.cancer.gov/statfacts/html/prost.html
[5] https://doi.org/10.1016/S0140-6736(24)00651-2
[6] https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.811044/full
[7] https://www.cancer.org/cancer/types/prostate-cancer/causes-risks-prevention/risk-factors.html
[9] https://www.cancer.org/cancer/types/prostate-cancer/detection-diagnosis-staging/signs-symptoms.html
[10] Balk SP, Ko YJ, Bubley GJ. Biology of prostate-specific antigen. J Clin Oncol. 2003;21(2): 383–391.
[11] Lilja H, Ulmert D, Vickers AJ. Prostate-specific antigen and prostate cancer: prediction, detection and monitoring. Nat Revs Cancer. 2008;8(4):268–278.
[12] Catalona WJ, Partin AW, Slawin KM, et al. Use of the percentage of free prostate-specific antigen to enhance differentiation of prostate cancer from benign prostatic disease. JAMA. 1998; 279(19):1542–1547.
[13] https://www.cancer.org/cancer/types/prostate-cancer/detection-diagnosis-staging/how-diagnosed.html
[14] Kwon DH, Velazquez AI, de Kouchkovsky I. PSMA PET Scan. JAMA Oncol. 2022;8(12):1860. doi:10.1001/jamaoncol.2022.3531
[15] https://prostatecanceruk.org/prostate-information-and-support/prostate-tests/prostate-biopsy
[16] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469728
[17] https://www.news-medical.net/health/Types-of-Prostate-Biopsy.aspx
[18] https://www.cancer.net/cancer-types/prostate-cancer/stages-and-grades
[19] https://www.cancer.org/cancer/types/prostate-cancer/detection-diagnosis-staging/staging.html
[20] https://www.cancer.org/cancer/managing-cancer/treatment-types.html
[21] https://www.cancer.gov/about-cancer/treatment/types
[22] https://academic.oup.com/jnci/article/110/4/341/4430583
[23] Yordanova A, et al. Theranostics in nuclear medicine practice. Onco Targets Ther. 2017;10:4821-4828. doi:10.2147/OTT.S140671.
[24] https://doi.org/10.1002/cncr.28238
[25] https://www.bmj.com/content/371/bmj.m3503
[26] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6278096/
[27] https://meetings.asco.org/abstracts-presentations/230097
[28] https://doi.org/10.1007/s11912-023-01399-0
[29] https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet
1 The availability of products and solutions referenced here varies by country and depends on local regulatory requirements.

















