Home
Perspectives
- A closer look at neurodegenerative diseases
A closer look at neurodegenerative diseases
Neurodegenerative diseases are disorders characterized by the progressive degeneration of the structure and function of the central or peripheral nervous system.
These diseases occur when neurons lose function over time and ultimately die. Since there is no known way of reversing the progressive degeneration of neurons, these diseases are considered incurable.
What is a neuron?
Dementia and Alzheimer’s disease
Facts and Figures
Brain changes
Diagnosis
Disease management
Dementia causes symptoms that affect memory, thinking, and social abilities severely enough to interfere with a patient’s daily life.
What happens inside the brain?
Although there are many forms and causes of dementia, Alzheimer’s disease (AD) is the most common in older adults. The exact mechanisms of how and why various forms of dementia develop are still being investigated.
In Alzheimer’s disease, changes in the brain may begin a decade or more before cognitive decline is noticed. Abnormal deposits of proteins – amyloid plaques and tau tangles – form throughout the brain and prevent nerve cells (neurons) from communicating with each other. Healthy neurons stop functioning, lose connections with other neurons, and die. The damage initially appears to take place in the parts of the brain that are essential to forming memories. As more neurons die, other parts of the brain are affected and begin to shrink.
How is dementia and Alzheimer's disease diagnosed?
A lot of the diagnosis still depends on the report of relatives, who are often the first to notice changes in memory or personality and can describe changes over time.
Professor Clare Mackay, PhD, Associate Director, Oxford Centre for Human Brain Activity (OHBA), UK
Podcast episode
SPECT exams should be made more accessible by reducing costs. It would be useful for screening patients with cognitive risks, to protect both themselves and a healthy society.
Jun Hatazawa, MD, PhD, Chief Executive Director, Japan Radioisotope Association
The various forms of dementia are difficult to differentiate diagnostically. Physicians may
- ask the patient and caregiver about overall health, use of medicines, diet, past medical problems, ability to carry out daily activities, and changes in behavior and personality;
- conduct memory, problem solving, attention, counting, and language tests;
- order standard medical tests, such as blood and urine samples, to identify other possible causes of the symptoms;
- use magnetic resonance imaging (MRI) to visualize changes in the brain, such as white and grey matter atrophy;
- order positron emission tomography (PET) to visualize amyloid and/or tau deposits;
- perform lumbar puncture, in which a small sample of cerebrospinal fluid – which surrounds the brain and spinal cord – is removed from the spinal canal for laboratory analysis for amyloid and tau molecules.
Physicians might repeat these tests to gain information about how the patient’s disease is developing over time.
The likelihood of developing Alzheimer’s may be only one to two percent at age 65. But then it doubles every five years. Existing drugs cannot reverse the course of the degeneration, they can only slow it down. This is why it’s crucial to make the right diagnosis in the preliminary stages – when the first mild cognitive disorder appears – and to filter out Alzheimer’s patients.”
Andreas Papadopoulos, MD, PhD, Scientific Coordinator, Iatropolis Medical Group, Athens, Greece
Increased image contrast and high resolution enable the identification of small anatomical structures and the clear differentiation between gray and white matter and cerebrospinal fluid.

The images show decreased perfusion in the frontal and parietal lobes bilaterally, while the central sulcus areas are relatively spared. Alzheimer’s disease is suspected.
What is the central sulcus?
Can dementia and Alzheimer's disease be treated?
Unfortunately, there is currently no cure for Alzheimer's disease. However, certain treatments like behavioral therapy and medication can help ease the symptoms of the disease, and starting treatment early may help preserve daily functioning for some time. In addition, early diagnosis will allow families to take care of financial and legal matters, address potential safety issues in the patient’s surroundings, adapt the person’s home, and develop support networks.
Podcast episode
Parkinson‘s Disease
Facts and Figures
Brain changes
Diagnosis
Disease management
Parkinson signs and symptoms can be different for every patient. Early signs might be mild and can even go unnoticed.
What happens inside the brain?
Two pathological changes are regarded as hallmark signs of Parkinson’s disease. The first is the breakdown and death of dopamine-producing cells in the substantia nigra. The substantia nigra is one of several structures in the brainstem that make up the basal ganglia, which is extremely important for movement. Scientists still do not know what causes these cells to die, but when dopamine levels decrease, it causes abnormal brain activity that leads to impaired movement and other symptoms of Parkinson’s. By the time a Parkinson’s disease patient dies, they may have lost up to 70 percent of the dopamine neurons in this region. As the disease progresses, neurons in other areas of the brain and brainstem begin to die as well.
Researchers have also noted the presence of Lewy bodies, which are clumps of specific substances within brain cells. Among the substances contained in Lewy bodies, scientists focus on a protein called alpha-synuclein (a-synuclein). It is found in all Lewy bodies in a clumped form that cells cannot break down.
What is dopamine?
Dopamine is an important neurotransmitter in the brain. It plays a key role in motivation- and drive-increasing effects. If dopamine levels are too low or too high, Parkinson's-like or mania-like symptoms may occur.

Substantia Nigra
Normal (left), Parkinson's disease (right): Computer illustration showing healthy substantia nigra and degenerated substantia nigra in the human brain. The substantia nigra plays an important role in reward, addiction, and movement.
How is Parkinson’s diagnosed?
No specific laboratory or imaging test can conclusively diagnose Parkinson’s disease. However, because several other disorders can cause similar symptoms, it is important to arrive at a diagnosis as soon as possible. The diagnosis is based on a patient’s medical history, a review of their signs and symptoms, and a physical and neurological examination. The physician may also order laboratory or imaging tests to rule out other conditions.
A single-photon emission computed tomography (SPECT) examination – called a dopamine transporter (DaT scan) – can support the suspicion of Parkinson’s disease. However, it is often only possible to confirm a Parkinson’s disease diagnosis once Parkinson’s disease medication has been initiated and the patient has significantly improved. Frequently, it takes time to diagnose Parkinson’s disease. Physicians may recommend regular follow-up appointments to evaluate the patient’s condition and symptoms over time.
With objective assessment, we can predict the occurrence of movement disorder, which is useful for the prevention of Parkinson’s disease.
Hiroshi Matsuda, MD, PhD, Director, Cyclotron and Drug Discovery Research Center, Southern Tohoku Research Institute for Neuroscience, Japan

A normal SPECT DaT image (top) with the corresponding MR image (bottom). While DaT imaging is normally done with SPECT/CT, the striatum is better localized on MR images.
Can Parkinson’s be treated?
At present, there is no cure for Parkinson’s disease, but a variety of medications provide considerable relief from the symptoms. Treatment for each patient is based on their individual symptoms. Medications can help control and often significantly improve symptoms, but they cannot reverse the effects of the disease. The medications include
- drugs that increase dopamine levels in the brain;
- drugs that affect other brain chemicals;
- drugs that help control symptoms that are not movement-related.
Over time, however, the benefits of the drugs frequently diminish or become less consistent.
Additional treatments involve physical, occupational, and speech therapies that help with movement and balance disorders, tremors and rigidity, decline in mental function, and speech problems. Other supportive measures include a healthy diet and getting more rest.

In some more advanced patients with unstable medication responses, deep brain stimulation (DBS) surgery may be advised. This involves implanting electrodes into a specific part of the patient’s brain and connecting them to a small generator implanted in the chest. The device and electrodes painlessly stimulate the brain to block signals that cause many of the movement-related symptoms of Parkinson's – such as tremor, slowness of movement, and rigidity. Although DBS may provide sustained relief from symptoms, it doesn't keep Parkinson's disease from progressing and some symptoms may gradually return.
Multiple Sclerosis
Facts and Figures
Brain changes
Diagnosis
Disease management
Multiple sclerosis is a disease with unpredictable symptoms that can also vary in intensity. Different symptoms can manifest during relapses or attacks.
What happens inside the brain?
Multiple sclerosis (MS) is an autoimmune disease. The body’s own immune system attacks the myelin sheaths that cover and protect the axons. These nerve fibers connect nerve cells within the central nervous system (i.e., the brain and spinal cord). Axons are like cables, and the fatty myelin sheaths insulate them.
When this insulation is destroyed, the nerves’ ability to conduct electrical and chemical signals becomes slower, uncoordinated, or entirely nonexistent, depending on the severity of the damage. Over time, the uninsulated nerve fibers themselves, and even whole nerve cells, die. This leads to brain atrophy. Damage to specific brain regions can make it hard to perform specific skills located in that region. There are two forms of multiple sclerosis : in relapsing-remitting multiple sclerosis, patients have periods when symptoms flare up, and periods when they calm down; in progressive multiple sclerosis, the symptoms get steadily worse.
What does atrophy mean?
How is multiple sclerosis diagnosed?
There is no single test for multiple sclerosis; a combination of tests is used to rule out other diseases that may cause similar symptoms and to diagnose multiple sclerosis. After taking the patient’s medical history and physical examination, a physician might order the following tests:
- Blood tests are currently mainly used to rule out other diseases with similar symptoms, although research is under way to also detect MS-related biomarkers in the blood.
- Magnetic resonance imaging(MRI) is used to detect damage or scarring of the myelin sheaths in the brain and spinal cord.
- Lumbar puncture involves removing a small sample of cerebrospinal fluid – which surrounds the brain and spinal cord – from the spinal canal for laboratory analysis. This sample can show abnormalities in immune cells and antibodies that are associated with MS.
- Evoked potential tests measure the minute electrical signals that occur in certain areas of the brain in response to stimulation, such as from sound, touch, or sight. They can be measured by electrodes placed on the scalp.
Physicians can repeat these tests to gain information about how the patient’s disease is developing over time.

7-tesla-imaging for early detection of MS
How to accelerate progress in diagnosis and treatment
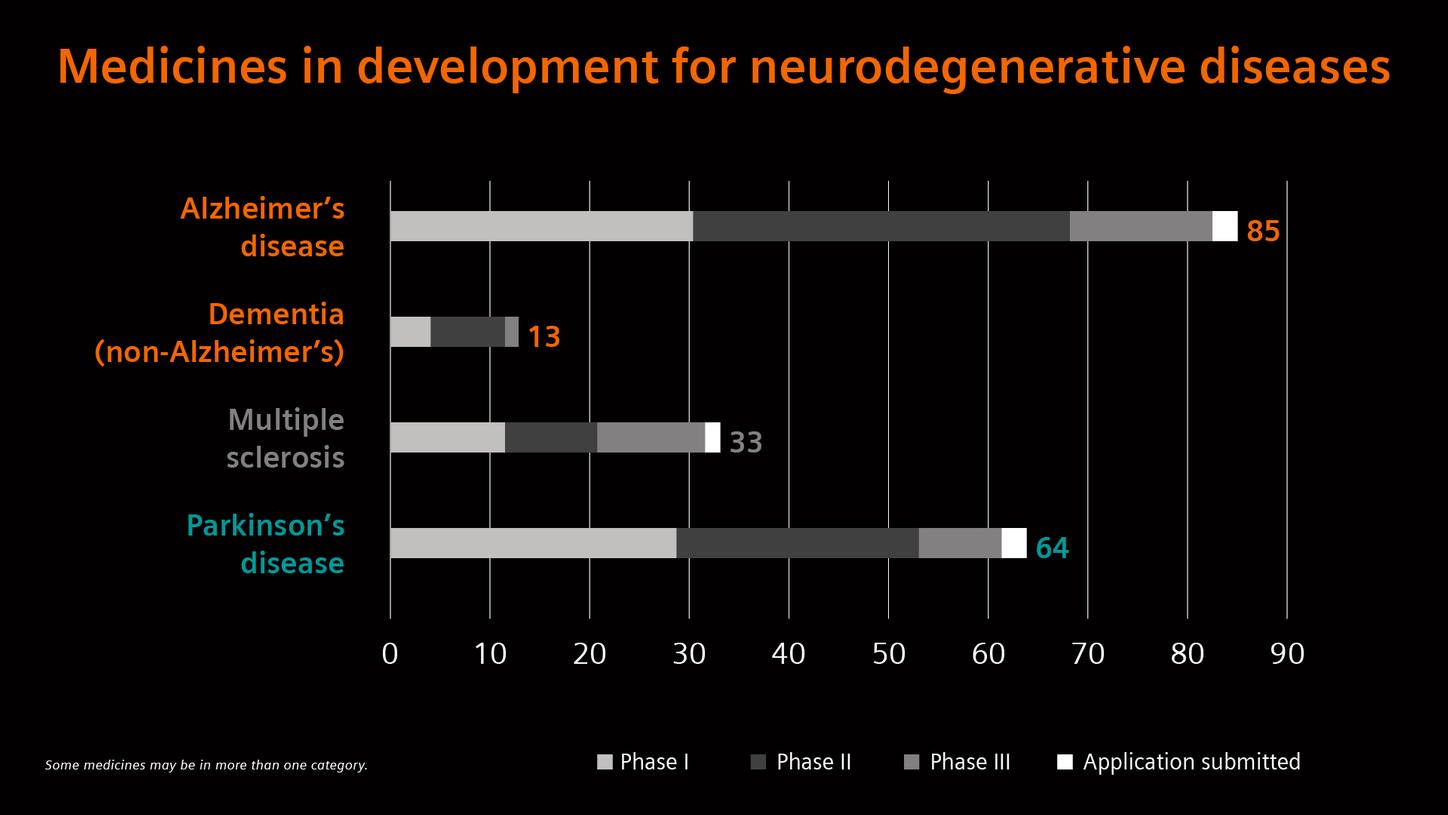
Given the limited diagnostic and therapeutic options for neurodegenerative diseases, researchers, and industry are pooling their strengths.
Podcast episode
What lies ahead?
Looking at the near future - what could be possible next steps and developments?
The disorder starts 20 years before you see the symptomology. So, people have started to generate studies of healthy people, and follow them in time to identify early biomarkers. If you find the biomarker, or molecules in the blood, that reveals the first signs of the disease, you can try the drugs right away. Until we reach that point, it will be very difficult to find drugs.
Professor emeritus Adriana Maggi, PhD, University of Milan, Italy
Biomedical research has revealed many similarities between neurodegenerative diseases, including atypical protein accumulations and induced cell death. These similarities suggest that therapeutic advances against one neurodegenerative disease might improve therapies for others as well. Most of today’s medications only treat the symptoms, which provides some relief to patients, but does not prevent the disease from progressing. Disease-modifying therapies (DMTs), which can create a lasting effect on the trajectory of clinical and cognitive decline, are needed to address the underlying causes of these diseases. But progress has proven challenging.
Scientific complexities in neurodegenerative diseases include getting medicines across the blood-brain barrier, finding appropriate animal models that can inform human efficacy, a lack of validated molecular targets for drug development, and a lack of well-defined biomarkers that can help measure consistency of treatment effect in clinical trials.[11] Additionally, many neurodegenerative diseases are heterogenous conditions with multiple root causes that make it difficult to diagnose patients, identify treatments, and predict how individual patients will respond to it.
1 Disability-adjusted life years (DALYs) measure overall disease burden, expressed as the number of years lost due to ill health, disability, or early death. They are also used to measure the impact of single diseases on a population.
2 Research mode on MAGNETOM Terra is still under development and not commercially available in the U.S. and other countries. Its future availability cannot be ensured.
The images are acquired with a MAGNETOM 7T which is for research only. All data shown are acquired using a non-commercial system under institutional review board permission.
The statements by Siemens Healthineers customers described herein are based on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist (e.g., hospital size, case mix, level of IT adoption) there can be no guarantee that other customers will achieve the same results.All sources last accessed May 15, 2021
[1] https://www.alzint.org/about/dementia-facts-figures/dementia-statistics
[2] https://alz-journals.onlinelibrary.wiley.com/doi/abs/10.1002/alz.042236
[3] https://www.alzint.org/about/dementia-facts-figures/dementia-statistics
[4] https://www.parkinson.org/blog/raise-awareness/10-Interesting-Facts-About-Parkinsons
[5] https://parkinsonsnewstoday.com/parkinsons-disease-statistics[6] https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(18)30295-3/fulltext
[7] https://www.parkinson.org/blog/research/economic-burden-study
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7720355
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3770174
[10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5476197/
[11] Gribkoff VK, Kaczmarek LK. The need for new approaches in CNS drug discovery: Why drugs have failed, and what can be done to improve outcomes. Neuropharmacology, 1 July 2017, volume 120
[12] Myszczynska, M.A., Ojamies, P.N., Lacoste, A.M.B. et al. Applications of machine learning to diagnosis and treatment of neurodegenerative diseases. Nature Reviews Neurology, 15 July 2020, volume 16
[13] Medicines in development. 2021 report: neurodegenerative diseases. Pharmaceutical Research and Manufacturers of America. 12 October 2021




























